|

中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
中文首页
英文版1
参考文献1-150
参考文献511-1048
|
|
'Acupuncture is a placebo'? Are you kidding?
- Errors
and mistakes in acupuncture researches in Western countries (II)
Dr. Martin Wang, MD. Ph.D.
Registered Acupuncturists
Edmonton, Canada
|
|
Chapter 6. The ability of an acupuncturist
6.1. Length to have an acupuncturist license
does not represent the personal clinic skill of
an acupuncturist
6.2.
Stress of acupuncturist in acupuncture study
6.3.
Choose of acupuncturist to participate in an
acupuncture study
Chapter 7. Similarities and differences between
acupuncture studies in China and in the Western
world
7.1. Design of studies
7.2. Operators of acupuncture treatments
7.3. Use of pain killer during study
7.4. Sources of patients in a study
Chapter 8. Why the acupuncture healing effects
could be better in acupuncture clinic than in a
study
Chapter 9. The direct evidence that acupuncture
is not a placebo effect
9.1. Acupuncture in the treatment of coma
9.2. Acupuncture in the treatment of shock
9.3. Acupuncture in persistent vegetative state
9.4. Acupuncture before and during anesthesia
9.5. Acupuncture during general anesthesia
9.6. Acupuncture in delayed wake-up after
general anesthesia
9.7. Acupuncture anesthesia in shock patients
9.8. Acupuncture in dementia
9.9. Acupuncture-induced anesthesia or
acupuncture-combined anesthesia
Chapter 10. Different healing effects with
different ways of acupuncture
10.1. Different acupuncture points
10.2. Acupuncture points versus non-points
10.3. Different needle-manipulation technique
10.4. Acupuncture versus sham acupuncture
Chapter 11. More examples supporting that
acupuncture are not merely a placebo
11.1. Acupuncture in children
11.2. Acupuncture in animal
Chapter 12. Why some researchers could feel that
acupuncture is merely a placebo effect
12.1. The healing effects of acupuncture group
and sham group are pretty close in the studies
in Western countries
12.2.
Comparing between different treatment frequency,
between different acupuncture points, between
acupuncture points and non-points, between
different technique, no significant difference
12.3. Simply contribute the most part of the
healing effect in the acupuncture group into a
placebo effect, only a small part into the
acupuncture specific effect
12.4. Improperly choose acupuncture points,
contribute its low effect to that of acupuncture
12.5. Study on a disease that is not in the
working scope of acupuncture treatment
12.6. Confuse the healing effect of cupping,
moxi, electrical acupuncture, auricular
acupuncture, TENS, massage, all as acupuncture
12.7. Superstitious belief on large scale
experiments
12.8.
Co-exit of opposite ways in acupuncture
treatment
12.9. Not care or omit large amount of positive
results
Chapter 13. Arguments among researchers and in
the internet world
Chapter 14. Opinions and comments from Chinese
acupuncture community
Chapter 15. Our own opinion and suggestions
about acupuncture research
15.1. Selection of acupuncturist in study
15.2. Special acupuncture study
15.3. Ordinary acupuncture study
15.3.1. Pre-test phase
15.3.2. No-treatment group
15.3.3. Sham group
15.3.4. Acupuncture group
15.3.5. Location of study
15.3.6. Supervisor
15.3.7. Recommended acupuncture experts or
masters
15.3.8. Multiple research location versus single
location but more clients
15.3.9. Aim and goal of the acupuncture study
for the current time
Chapter 16. Specificity of acupuncture study
Chapter 17. Summary
Chapter 18. Explanations about this article
Chapter19. Consideration and suggestion for
future medical service system
Chapter 20. Letter to editors
Chapter 21. Comments and suggestions from
readers
Footnotes
References
Chapter 6: The ability of an acupuncturist
6.1. The length of license does not represent clinic skill
of acupuncturist
Colquhoun D
noticed that the positive articles about acupuncture come
mostly from mainland of China, Taiwan, Hong Kong, and Japan,
and so on. We also noticed that the negative articles mostly
come from Western countries and from the hands of physician
or physiotherapists. In such Western articles, the healing
effect of acupuncture in acupuncture groups is about 30% to
40% higher than no-treatment groups, and about 10% to 15%
higher than sham acupuncture groups. Such healing effect is
much less than our own clinic efficiency, and also much less
than the reports from China or other parts of Asian
countries.
The ability of an acupuncturist is
not determined by how long time the person hold acupuncture
license, or where the person get acupuncture training. These
should not be the absolute parameters to tell the clinic
skill of an acupuncturist. We believe that, the
acupuncturist in an acupuncture research should be the one
of higher level of clinic skill. It would be better if the
acupuncturist is recommended by Acupuncture associations.
Acupuncture is a profession of highly personal skill
dependence. It does not mean that high academic level or
longer education in acupuncture would ensure the higher
clinic skill.
In the Western countries, some physiotherapist,
chiropractic, or physician, can also get the license for
acupuncture after taking part in acupuncture training for
some time. For example, a physician has an acupuncture
certificate after 140 hours training would be allowed to
participate acupuncture study.
Some
times, even new graduated students can participate the
research.
,
In
review the acupuncture studies in the Western countries, it
seems that anyone may act as an "acupuncturist"
in the study, if they get hundreds of hours of acupuncture
training and get acupuncture license for some years. It
seems that they feel that, to practice acupuncture, it is
already enough if they choose the acupuncture points used by
other researchers, and if they indeed induced the Deqi
needle sensation. Under this condition, whether the results
are positive or negative is the credit of the acupuncture,
nothing related to their own level of skill in acupuncture.
The acupuncturists in China who participate the acupuncture
study is ensured by their published articles. Their articles
would not at all be accepted for publish, if their
acupuncture study cannot improve the healing effect of
current acupuncture technique, or if their work does not
allow better understanding of acupuncture mechanism or other
aspects of acupuncture. However, any articles about
acupuncture can be published in the Western countries, if
the article meets the need of some basic requirements for
the publication, such as randomization, blindness, with a
sham acupuncture group, or a waiting group, more than 20 to
30 patients in each group, and statistically analysis of the
data. To the view of acupuncturists in China, they learned
almost nothing from so many published articles from Western
countries.
If
we do not pay attention to the personal skill
of acupuncturist, no any acupuncture studies of best design
would reach truth. Such as to let a new person shoot a gun,
the best gun does not ensure that the person would shoot to
the target.
Unlike medical research in Western medicine, which mostly
studies uniform of chemical tables, any study involving
personal skill, such as acupuncture, massage, chiropractic,
physiotherapy (if it is manual therapy), needs to choose the
highest level of practitioners to take part in. We cannot
just pick up a student infighter from US school to match the
infighter of national level in Tailand. If the US infighter
lost, can we say that US infighter level is lower than that
of a Tailand infighter?
White P (2012)
had a study of acupuncture for the treatment of
osteoarthritic pain. The study
involved three acupuncturists. The healing effects of
the three practitioners are 37%, 17% and 62%. Though it
was explained by the author that the highest healing
effect by the third acupuncturist might be due to the
impression of him by patients more professional and more
like an expert, it cannot exclude that his personal
skill in acupuncture might be really highest. No matter
what could be the reason, the huge difference in the
healing effects by the three acupuncturists will affect
the data analysis for sure. It is possible that to
compare the healing effect by the third acupuncturist
with sham acupuncture, it would show statistically
significant difference
(63% vs 28.4%, or 63% vs 39.2%), rather than no
difference as reported.
Hawk C (2002)
reposted their chiropractic study on chronic pelvic pain.
The study involved 3 clinic locations. After 6 weeks of
chiropractic treatment, the pain level reduced by
59.1%,26.9%,84.6%,
in the three locations, respectively, average of 56.6%,
while the reduction rate in sham group is 68.5%. The healing
effect of the treatment group is even less than the sham
group! The practitioners in the 3 clinic locations were
reported to have 20, 10 and 12 years of clinic experience.
Having no alternative but the author have to admit that "The
technical and personnel resources required to achieve
adequate standardization of procedures at multiple sites may
make a placebo-controlled trial unfeasible, given our
current lack of knowledge about the active agent in manual
chiropractic procedures. It might be more efficient to
reverse the traditional order of experimentation used for
pharmaceuticals, which begins with safety, proceeds to
efficacy and finally to effectiveness. Because
chiropractic—a CAM profession using manual methods for more
than 100 years—can scarcely be considered in the same
category as a newly developed medication, it might be
reasonable to first investigate effectiveness. If
chiropractic care that is provided by experienced
chiropractors who are allowed to use their best clinical
judgment of how to apply the procedures is documented in
such studies to improve patient outcomes compared to
standard medical care alone, more in-depth and controlled
studies would then be warranted to identify specific aspects
of that gestalt of care that are most responsible for
the outcomes or if there are certain subpopulations of
patients who benefit most from them."
Apparently, it is not reliable to tell the personal skill of
chiropractic practitioners by license holding time, neither
of acupuncturist.
Forbes A
reported their acupuncture study. Acupuncturist A treated 12
patients with IBS, 50% patients had the symptom level
reduced by 4. Acupuncturist B treated 15 such patients and
33.3% of patients had the symptom level reduced by 4. The
author had no alternative by to combine the data together,
so as to reduce the unlikelihood of the study conclusion.
So, for these of large scale clinic researches involving
many clinic locations and many practitioners, how high level
of the creditability for their study conclusion?
Another
example is from report of
Deng
G
(2007)
for the treatment of hot flash by
acupuncture. During the study, the acupuncturist was changed
and the reduction curve of the hot flash even reversed up.
They had acupuncture twice a week for 4 weeks. The hot flash
reduced by about 30% to 35%, similar to that in sham group.
Fregni F (2010)
pointed out, in an international placebo symposium working
group, that "a great number of
interventions used in PRM depend on the technician’s or
clinician’s skills such as the application of acupuncture,
injections, and nerve blocks. Therefore, controlling for
these interventions becomes difficult with this important
source of variability. This makes it even more difficult to
design an appropriate placebo in these situations. To
control for skills and levels of experience, it would be
necessary to conduct multicentric studies with various
levels of skills and experiences and perform multivariate
analyses to adjust for these variables. In this scenario, a
large number of patients would be necessary, increasing the
difficulties to conduct such studies."
If the personal skills among several acupuncture operators
are so different, how can we trust the stuy involving 67
physiotherapists,
122 physician,
or 320-340 physician?
As pointed out by Forbes (2005)
that the possibility that
simplified acupuncture as delivered by
Western-medicine-trained acupuncturists might have given a
different result is intriguing and may warrant further
study.
6.2. Additional issue for acupuncturists in acupuncture
studies
Of course there is another possibility that the acupuncture
in a study is requested by acupuncture researcher, not
accepted by the acupuncturists themselves.
The acupuncturists in an acupuncture study may suffer from
emotional stress, that may affect their perform of
acupuncture treatment.
McManus CA
(2007)
have dad a survey to the acupuncturists in thir acupuncture
study. They send surveys to 12 acupuncturists and get 8
responded.
They reported that “all
respondents reported feeling challenged by their work as
investigators as opposed to their “normal” roles as
clinicians. Although all agreed that the protocol was
reasonable at the outset, in particular, they still felt
strong urges to apply the typical tools of their clinical
practices such as active needling, heat, external herbal
treatments, treatments for the “whole” person, and
counseling. (To our best knowledge, none of them acted on
these urges.) During monitoring interviews, many
acupuncturists indicated how difficult it was not to be
permitted to offer dietary, ergonomic, or physical advice to
the participants. Several acupuncturists reported that they
frequently hoped that participants would be randomized to
the genuine acupuncture group after the placebo run-in had
been completed. In one instance, an acupuncturist actually
called the clinical coordinator and requested that a patient
be re-randomized to the genuine treatment group. Unwilling
to comply with the rigors of RCTs, this acupuncturist (whose
responses are included here) was not assigned to treat more
participants in the study.
Although 12 acupuncturists were originally trained for
the RCT, 5 did not stay with the trial for its entire
course. Study coordinators ceased assigning participants to 3
acupuncturists because they broke the protocol (e.g., for
using nonprotocol points in the active phase, failing to keep
accurate records, or for being unclear about the study’s
procedures.) Two (2) other acupuncturists resigned from the
trial: 1 because of the ethical concerns with administering
the sham treatment and the other because of re-locating out
of the state.”
Apparently, the
mode of acupuncturists in an acupuncture study could be
different from their routine clinic work. Could this unstable
emotion condition of acupuncturists
affect the acupuncture efficacy?
6.3. Selection of acupuncturist for acupuncture research
Certainly we should not carelessly image, as others,
the level of personal skill of any acupuncturists.
We propose a preliminary idea for the selection of
acupuncturist for acupuncture study:
Basic selection: the acupuncturist should have a
comprehensive healing effect for most of diseases in his/her
clinic as high as 75% (within one to two months). The
comprehensive therapies mean the use of acupuncture,
cupping, moxibustion, bleeding therapy or whatever commonly
used therapies in an acupuncture clinic.
It should not be difficult to find such acupuncturists.
Specific selection: the acupuncturist should have at least
75% of an average healing effect (as published data, for
example from China) for the disease/symptom to be studied,
when only the acupuncture was used in a pilot study. The
average healing effect by acupuncture is different for
different disease/symptom. For example, if an average
healing effect for non-specific low back pain, treated by
acupuncture alone, reported from China, is 55%, the healing
effect of the candidate acupuncturist for the same kind of
low back pain should be more than 41%.
The reasons for the basic selection is: if the acupuncturist
cannot reach such healing effect with their own natural
matter, it would be impossible for them to create a positive
result in a Western style of acupuncture study
[16],
in which only acupuncture, not moxi, not cupping, or any
other kind of therapies, are allowed. What is the use to
create so many negative data by untrustable ways of studies?
The reasons for the special seletion is that
even if the acupuncturist passes the basic selection, it
still does not mean that he or she is able to treat the
disease to be studied. For example, if an acupuncturist
never treated coma patients (due to stroke), it would be
hard to believe that the acupuncturist can treat such
patients in a study.
If there is no any people passes such selections, it would
mean that the conditions for an acupuncture study are not
met. The acupuncture study should not be started. Can any
surgeon perform a craniotomy without anesthesia by an
anaesthetist?
The ability of the acupuncturist can be tested in a pilot
study or in a large scale study with a free-treatment group,
in which the acupuncturist can treat the patient by whatever
his natural way. If the healing effect in the free-manner
could not exceed 45% ,[17]
it is ready to tell that the study fails at least because
the poor skill of the acupuncturist. Before the study, the
researcher should ask the acupuncture if the acupuncture has
confidence for the disease to be studied by acupuncture. If
the acupuncture said yes, then the researcher would mean
"show to me".
In the acupuncture study, we should not only pay attention
to the diagnosis of the disease to be studied, the selection
of patients, randomization, blindness, or cross-group, such
organizing issue, but also the quality of an acupuncturist.
Brief summary:
The personal skill of an acupuncturist is one of the most
important factors determining the success of an acupuncture
study. It is needed to set up a role for the selection of an
acupuncturist for an acupuncture study.
Chapter 7. Similarity and difference between acupuncture
studies in and out China
There are several differences between the acupuncture
studies in and out of China, beside what we have discussed
above .
7.1. Design of study
For acupuncture study in the Western countries, the so
called high quality studies means: randomization, blindness
(single or double), with sham group (plus waiting group). If
there is a sham group, it is better to also have a cross
design.
If there is no waiting group, it would be hard to exclude
natural regress of the disease from the sham group. This
might be true since the acupuncture studies in the Western
need a long time to finish, up to 1 to 2 years. A disease
might get better by itself. With a sham group, it would be
not so ethical to "cheat" patient, so a cross design was
used and the patient initially in the sham group can be
later treated with real acupuncture.
Actually, no matter for acupuncture or for Western medicine
or surgical studies in Western countries, only little studies
met these standards. Most of acupuncture studies do have
randomization, blindness, using Western medicine as control
group but no sham group or no waiting group (no-treatment
group). The presumption of such design is that the healing
effect of the control group (Western medicine group) have
been tested to be effective by "strict" randomization,
blindness, compared with sham group. Therefore, if the
healing effect of acupuncture group is equal to, or higher
than, the control group, the healing effect of acupuncture
group should be accepted. This is true especially for the
treatment of some difficult diseases, for which the current
Western medicine shows some effectiveness but also terrible
side effects.
Unfortunately,
this presumption might not be true. The medicine in the
control group may not be tested by the "strict" studies at
all. It is not a long time that FBA of US asked a new
medicine to compare with a sham group. Many medicine are
still in use for a long time though they have never been
tested comparing with a sham. It may cause an
uncertainty to compare acupuncture with such non-tested
medicine. Secondly, someone might ask if the placebo effect
in the medicine group and in the acupuncture group are not
the same level.
The acupuncture studies in China mostly have also a
randomization, but compared with Western medicine, or
compared with other type of acupuncture technique. Rarely
there is blind design, or a sham group. This might be
because the acupuncturists in China do not believe their own
acupuncture could be a placebo effect. The data we could
collect (Fig. 20a, 20b, 20c, 20d) appear to support their
confidence.
Because the healing effect of acupuncture group is only 10%
to 15% higher than the sham group, after analyzed by
statistic, the dada are easy to loss significant.
Acupuncturists in the Western did not realize that it is due
to the low healing effect of the acupuncture group, but to
an improper sham group. So, they have paid much attention to
modify the sham group and study the mechanism of the placebo
effects. While acupuncturists in China do not believe that
acupuncture could be placebo effect, and they do not believe
that to insert needle to a non-point could result in a
higher healing effect than insert the needle into typical
acupuncture points. So, they usually use inserted needle
(into non-point) as sham group. In such sham, the sham
needle is even inserted the same depth as real acupuncture
group. (see Attached list
19a,19b,
19c).
Acupuncture study in the West ern uses sham treatment. This
cause a ethical problem. It is therefore needed to tell the
patient that he or she might be allocated into a sham group,
or a new treatment group and so triggers patient expect for
healing. Researchers have to try to bind the patient from
which group he was allocated, to eliminate the communication
between the acupuncturist and the patient, to design a cross
design, all of which increase the complex of the study and
also largely "modified" the real acupuncture treatment
course. For this reason, we would say that the acupuncture
study in the west is an "modified" acupuncture, not a real
one.
The healing effect of acupuncture in China is usually more
than 40% to 50%. The aim is to test if a new way of
acupuncture (Chinese modified acupuncture) would work better
than currently used ordinary acupuncture. Generally
speaking, the effectiveness of the modified acupuncture is
usually 50% to 65%, better than the ordinary acupuncture.
The paper would not be published if the effectiveness of the
modified acupuncture is no more than ordinary acupuncture.
That means, acupuncture study in China is to find better and
higher efficient acupuncture, not to test if acupuncture is
a placebo effect. Therefore, acupuncturist can learn from
the modified acupuncture to update their technique again and
again.
When there is a sham group in acupuncture study in China,
the needle is inserted. Current data (Fig.20a, 20b, 20c,
20d) showed that, with higher treatment frequency, the
healing effect of acupuncture group is much higher than the
sham group. This makes it not important to use either
inserted or not inserted needle in the sham group. So, it is
not needed to blind the patients. The healing process would
be much less complex than that in Western studies.
Acupuncture study in China is to compare the healing effect
of the modified acupuncture with ordinary acupuncture. Why
we cannot regard the ordinary acupuncture as also a sham? In
this way, we do not need to specifically design a sham
group, no need to tell patients that they may come into a
no-real treatment group, so no need to design a cross study,
because the patient will get either a ordinary acupuncture
as usually for any other patients, or an even better way of
acupuncture. We did not interrupt the patient expectation at
all.
Acupuncture study in China usually takes a short time to
finish (2 to 3 months). For a chronic disease and due to
many years of clinic experience that the disease cannot get
30% to 50% improvement without proper medical help, so that
the 30% to 50% improvement in the acupuncture group is not
regarded as natural regression, so no need to have a
non-treatment group as a control.
7.2. Acupuncture operator
In the acupuncture studies in the Western, many times the
acupuncture was performed by physician, next by
physiotherapist. If we make a summary from Attached list 14,
we can see that, half of the performers are acupuncturists,
one third is physician, 12% is physiotherapist
(Fig. 21), e.g. half by acupuncturists and another half by
non-acupuncturists.
It is quite common that we have clients come from
physiotherapy or chiropractic clinic. According to the
story told by the patients, during the whole healing
course there, (more than 10 times), they got only 1 to 2
times of acupuncture treatments. Apparently these
practitioners still use their own original professional
way for the treatment and acupuncture is only some
complementary way in their clinic. While for the
acupuncturists in China, they use acupuncture everyday
for all the patients in their clinic/department. They
have chance to reach lots of book/literature on
acupuncture to update knowledge, have chance to be
guided and supervised by top level experts. They can
have 60 – 100 patient every day (spend 20-30 min to each
patient).
It is clear for how rich their clinic experience could
be.
7.3. Use of pain killer
One of the apparent characteristics of acupuncture study in
the West is to allow the use of pain killer by patients
during the study. This is easy to understand: if the
acupuncture healing effect is not high enough, we cannot
stop the patients from the use of pain killer. If we have a
review of the data from
Colquhoun D
,Madsen
MV (2009),
and Vicker AJ (2012)
it can be seen that in total 22
articles, in 86.4% of the studies, the pain killer is
allowed to use.
In the articles published from China, it is usually not
indicated if the pain killer is allowed or not allowed.
However, due to higher treatment frequency and higher
healing effect, the symptoms were improved much faster and
patient most possibly no longer use the pain killer after
start of the acupuncture treatment. Our own experience
supports this presumption.
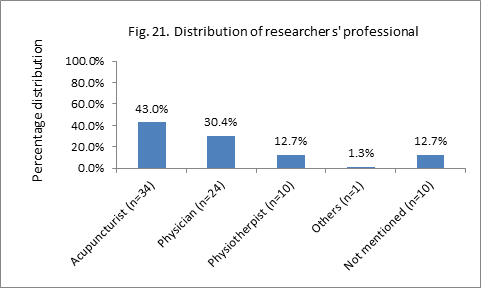
Fig. 21. n = experiment groups.
7.4. Sources of patients in study
Patients in the Western acupuncture studies mostly come
from an advertise.
This may create a higher expectation of patients to the
acupuncture
so to cause some level of placebo effect.
Also, most possibly, the patients do not need to pay for
the treatment, and they may give an exaggerated positive
comments to the treatment in the sham group and the
treatment group too.
The patients in acupuncture studied in China come by
themselves to the clinic. They are then allocated into
different groups by randomization. They do not know if they
are in an ordinary acupuncture group, or in a specially
modified acupuncture group, except if there is a sham group.
They need to pay for the treatment by themselves, so they
tend to give relatively more conservative comment to the
healing consequence. Many patients, when they see doctors,
no matter it is TCM doctor, acupuncturist, or a Western
medicine doctor, they tend to tell "I am still feeling
pain". While most of Western patients in our clinic tend to
say "better", or "though still pain, but better". They are
more optimistic than patients in China.
Though the patients in both the sham group and the
acupuncture group may give exaggerated positive comments,
because the healing effect of the acupuncture in the
acupuncture group is too low in these Western studies, the
extent of the healing effect in the acupuncture group is
only slightly higher than that in the sham group and it is
so easy to result in a negative result of the study.
Brief summary:
(1). Beside the difference in treatment frequency between
the acupuncture studies in the Western countries and in
China, there are some other differences between them, which
may also affect the study outcome.
(2). The acupuncture studies in the west emphasize the
randomization, blindness, sham group as a control group. The
aim is to test if the acupuncture effect is a placebo
effect. The acupuncture studies in China are mostly
comparing special or modified acupuncture technique with
Western medicine or with ordinary acupuncture. The aim is to
find more effective ways of acupuncture treatment, or to see
if acupuncture can be a better alternative therapy to the
conventional medicine: same or higher healing effect and
less side effect.
(3). The operators of acupuncture treatment in the
acupuncture studies in the west is half acupuncturists and
half non-acupuncturists. The personal skill of these
practitioners are unknown. That in China is all most all are
acupuncturist. The personal skill is reasonable.
(4). In the acupuncture group in the Western studies, the
patients are still taking pain killer, so affecting the
evaluation of the healing effect. In that in China,
patients may not continue the use of pain killer soon after
the start of the study, so the result of evaluation of
healing effect is relatively more trustable.
(5). Patients in the Western studies come mostly from
advertising and no need for them to pay for the treatment,
so there is high chance for them to have higher expectation
to acupuncture, and give exaggerated positive comments to
acupuncture treatment. The patients in the studies in China
come mostly be the patients themselves, and have reasonable
level of expectation to the acupuncture and give reasonable
level of comment to acupuncture.
Chapter 8. Why the healing effect of acupuncture is higher
in clinic than in a study?
8.1. Acupuncture in a study in most time is a single form of
acupuncture
Acupuncture performed in an acupuncture study is usually
just the acupuncture per se. While the acupuncture in clinic
is usually combined with other therapies, such as
moxibustion, cupping, Guasha, Tuina, acupressure, auricular
acupressure, traction, bleeding therapy, bleeding-cupping
therapy, or electrical acupuncture, warm acupuncture, or
TENS, and so on.
8.2. Acupuncture in a study is a fixed manner
Acupuncture in a study is usually performed in a fixed
manner: fixed treatment schedule, fixed acupuncture points
selected, fixed numbers of needles, and fixed treatment
length, etc. with the aim to standardize the treatment
course, so as to reduce the variation of healing effect from
patient to patient. While the acupuncture in clinic is in a
flexible manner, it can be changed among patients, and
during the treatment for a given patients, the acupuncture
points, the number of the acupuncture points, the length of
each session, combined or not combined with other therapies,
etc. The aim of the flexibility is to make the acupuncture
treatment match the conditions of the patients: the
tolerability of patients to the needle stimulation, the
change of the severity of the disease, the life schedule of
the patients, the financial situation of the patients, etc.
Even for the acupuncture, we may use different acupuncture
points rather than those introduced in acupuncture text
book. For example, we may choose trigger points, start-end
point of a muscle group, and so on.
Sometimes, we may even combine the acupuncture with Chinese
herbal therapy, especially by those of acupuncturists who
come from China but now work in the Western countries, when
we feel that Chinese herbal therapy might work better than
acupuncture. In this case, the acupuncture treatment could
be a complimentary therapy to the herbal therapy.
8.3.
Acupuncture in a study is for a limited group of patients
Acupuncture study is performed usually to a given group of
patients: patients with the same diagnosis (Western medicine
disease category), and within a given severity of the
diseases, a given age of range, a given sex and so on.
However, the patients in clinic are largely variable. For
example, the patients with knee pain in clinic might belong
to different categories of arthritis, or sprain, or strain,
with various level of severity, various length of the
disease, and so on. Especially speaking, some diseases we
see their research from a study may not be seen in a clinic
often. For example in our clinic, most popular diseases we
see are various pain syndrome, poor sleep, stress, anxiety,
constipation, hot body or cold body (hands), menopause
syndrome, disorders in menstruation, infertility,
overweight, quit smoking, but very little of some other
kinds of diseases, such as cancer, AIDS, post-stroke
syndrome. We mentioned in the early of this article that our
clinic effectiveness could be up to 85%. This does not mean
that we can treat every kind of disease with such successful
rate.
All of these mean that, if it does not work for the
acupuncture in an acupuncture study, it does not mean that
the acupuncture in clinic neither work; or if the
acupuncturist in that study cannot improve the disease
condition, it does not mean other acupuncturist can not
either.
The acupuncturists in an acupuncture study should tell the
researchers what the difference is between the experimental
acupuncture and the actual acupuncture. It is not fare and
injustice to test the "artificial' Western style of
acupuncture and contribute its study results to clinic
acupuncture or Chinese style of acupuncture. If the
acupuncturist in the study tells that this is indeed their
own way of acupuncture in clinic, we would have to suspect
and question about the healing effect of acupuncture in
their clinic.
Brief Summary:
(1). The acupuncture used in an acupuncture study could be
different from that in a clinic.
(2). Acupuncture in an acupuncture study is a single form of
acupuncture, while that in a clinic is a combined therapies.
(3). Acupuncture in an acupuncture study is a fixed
manner, while that in clinic is flexible manner.
(4). The healing effect of acupuncture in an acupuncture
study may not be necessarily represent that in a clinic.
Chapter 9. Direct evidence that acupuncture is not a placebo
effect
9.1. Treatment of coma with acupuncture
It should have no argument that a placebo effect only
happens when a person is in a consciousness condition and
with a clear mind to able to analyze stimulations from out
side of the body. Now let us see how and if acupuncture can
be used to treat some special clinic conditions in which the
person is out of consciousness, such as coma, shock,
persistent vegetative state, anesthesia, etc.
For the treatment of coma patients with brain trauma and
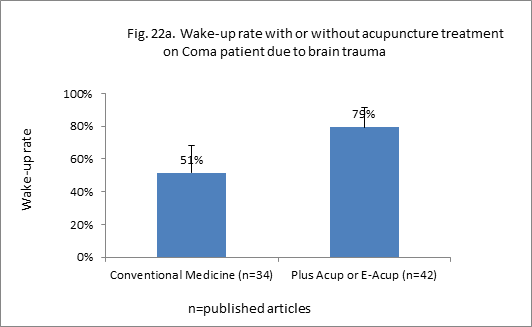
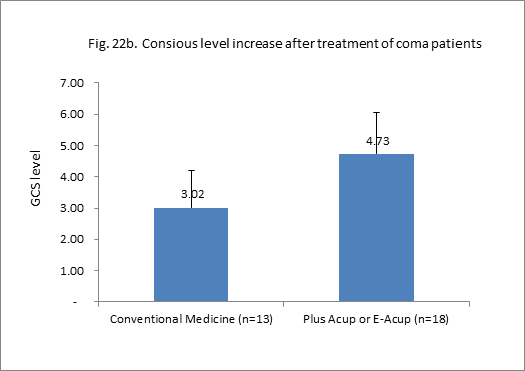
stroke, we collected about 40 articles.,
For such coma patients, acupuncture (Attached list
21a),
together with conventional rehabilitation therapies, can
speed up the wake-up rate from 51%±17%
increased to 79%±12% (Fig.22a), or to increase the degree of
consciousness (the GCS index increased from 3.02±1.2
to 4.73±1.3)
(Attached list
21b
,Fig.22b).
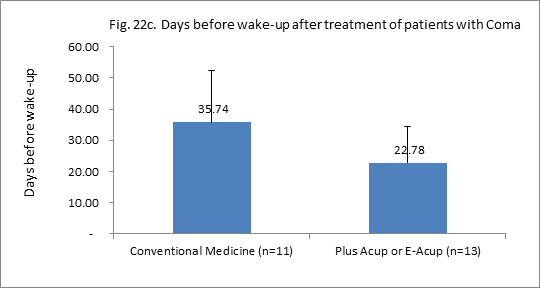
Or, it can be said that acupuncture treatment can shorten
the time needed to wake-up from 35.74±16.7days
down to 22.78±11.7
days (Attached list
21c,Fig.
22c).
Acupuncture alone can also reach such healing effect.
The combination of Western
conventional treatment with acupuncture treatment can no
doubt increase the cure rate and to reduce the sequela rate.
It should be pointed out that,
when acupuncture is used for the treatment of such severe
conditions, as coma, shock, persistent
vegetative state (see later), it is the modified acupuncture
that was used. The acupuncture treatment is at least once a
day. It would not be possible to reach such healing effect
if it is till performed once a week as current Western style
acupuncture.
蔡化理
(1961)
treated 27 patients with shock due to toxic dysentery.
Within 10-30 min of acupuncture, the blood pressure started
to increase. Only 2 cases needed blood pressure increasing
medicine.
9.2. Treatment of shock with acupuncture
Doctors in Second Affiliated Hospital of Hunan Medical
College (1973)
reported their way of treatment of shock for 160 cases.
Based on ordinary conventional ways, all cases were given
acupuncture treatment first. If the blood pressure did not
increase within 30 min, then started the addition of pressor
agent. By this way, blood pressure in 122 cases (76.3%)
clearly increased. The apparent effective rate was 76.3% and
total effective rate is 87.5%. This means that the blood
pressure in only 23.7% of patients did not respond to the
acupuncture treatment. This suggests that acupuncture
treatment has a function to increase blood pressure in shock
patients. These doctors found that for half of patients,
their blood pressure can start to increase within 30 min,
some after 60 min. There had been 9 patients, for whom the
use of pressor agent did not work satisfactory, after
addition of acupuncture, blood pressure increased in 8 cases
(systolic pressure up to 90 mmHg). This suggests that for
those cases whose blood pressure increase is not stable,
acupuncture can work to help the pressor agent. For some
patients, if the manipulation of the needles (by twisting)
stop for a longer time, the blood pressure would tend to
reduce. After stronger manipulation, the blood pressure
would increase again, suggesting that manipulation of needle
can influence the healing effect.
俞勤龙
(1997)
reported that doctors in the department of gynaecology and
obstetrics in the Jiangyin Hospital of traditional Chinese
Medicine treated 52 cases of shock patients after induced
abortion. The patients showed, during or after the
operation, pale face, cold hands and feet, palpitation,
press in chest, nausea or vomit, even reduction in blood
pressure, come, etc. The body condition became worse very
quickly and changed very fast. The blood pressure of the 52
cases all increased after stimulation of Sanyinjiao point
for several seconds. The patients then turned conscious to
recovery. No one case needed intravenous infusion or other
conventional emergency treatment.
宋智静
(1996)
treated 40 cases of shock patients due to allergic reaction
to penicillin by using acupuncture and epinephrine. For all
of the patients, after injection of epinephrine and
acupuncture on Neiguan point for 5 min, the face turned
pink, sweat stopped, consciousness turned back, blood
pressure increased, and pulse increases. The healing effect
showed as average 10 min (as fast as 5 min). Except for one
case who needed additional intravenous infusion and steroid
medicine, other 39 cases got recovered within 5 to 15 min.
No any death case. It can be commented that in this clinic
report, there is no control group to tell how much death
rate might be without use of acupuncture in the emergency
treatment. However, according to our own previous work
experience in emergency department in China, it has been a
very effective emergency treatment for those patients who is
already in a coma status, for the fact that their live were
saved within 5 to 15 min.
刘应柯
(1999)
and his colleagues treated hemorrhagic shock 33 cases
with acupuncture (no pressor agent). After half hour,
systolic pressure increased from average 62.6 mmHg to
average 98.3 mmHg. At the same condition, similar shock
patients 31 cases were treated without acupuncture (with
pressor agent). Their systolic pressure increased from
average 67.7 mmHg to average only 77.9 mmHg.
赵滨
(2008)
and his colleagues treated various kinds of shock 40 cases.
After acupuncture for 30 hour (no pressor agent), systolic
pressure increased from average 70.9 mmHg to average 95.6
mmHg. At the same condition for another 40 cases using
pressor agent (no acupuncture), systolic pressure increased
from average 68.9 mmHg to only average 85.5 mmHg. For
diastolic pressure in the acupuncture group, within half
hour treatment, it increased form average 42.3 mmHg to
average 58.7 mmHg. In the pressor agent group, it increased
from average 43.2 mmHg to only 55.24 mmHg.
傅立新
(2008)
treated various shock patients 138 cases. Within less than
30 min of acupuncture (no pressor agent), systolic pressure
increased from average 83.1 mmHg to average 101.1 mmHg.
Under the same condition with pressor agent use on another
138 shock patients, systolic pressure increased from 83.3
mmHg to 89.2 mmHg. In the acupuncture group and within less
than 30 min of acupuncture (no pressor agent), the diastolic
pressor increased from average 49.5 mmHg to average 59.3
mmHg. The diastolic pressure in the pressor agent group
increased from average 48.8 mmHg to 50.4 mmHg.
冀慧霞
(1999)
treated allergic shock 50 cases. With conventional emergency
treatment, the total effectiveness rate is 76%, while it is
90%, when the conventional way is combined with acupuncture.
The successfulness of acupuncture treatment is of course
also related to the intensity of the shock. The
effectiveness to low to mild level of shock is higher than
severe shock. It is also related to the type of shock.
Generally speaking, the effectiveness in allergic shock and
infective shock is higher, but that in cardiac shock and
hypovolemic shock, lower.
吴敬
(2000)
reported their treatment of cardiac shock, hypovolemic
shock, infectious shock and allergic shock with conventional
medicine plus acupuncture. The total effectiveness for these
different types of shock is 80%,82.6%,100%
and 100%, respectively.
张从道
(1989)
reported that, treated with acupuncture alone (no pressor
agent) for cardiac shock, the total effective rates for
hypovolemic shock, infectious shock, allergic shock, nervous
shock and traumatic shock are 90%, 95%, 93.3%, 95%, 93.3%
and 96%, respectively.
It should be noticed that acupuncture can not only work
together with pressor agent to increase the emergency
treatment of the
shock,
but also solve the emergency condition by itself alone.
Clinic
studies suggested that ,in
the treatment of shock with acupuncture, the blood pressure
increase occurs mostly within 30 min, while with pressor
agent, mostly after 3 hour. With acupuncture treatment, the
blood pressure increased earlier and higher. Especially it
happened in the earlier stage of shock. This is very
important to improve functions of important organs, such as
heart, brain and kidney, so as to prevent irreversible
damage to these organs.
To treat shock, every minute is very important to patient's
life. No time to allow us to have a sham group or a
non-treatment group. It should be accepted to compare
acupuncture-alone group and the acupuncture plus pressor
agent group, e.g. to compare conventional treatment with or
without acupuncture. Studies here all tried half hour of
acupuncture first. If the blood pressure does not increase,
it is added right away with pressor agent. The results
showed that combination with acupuncture worked much better
than without acupuncture. Indeed sham acupuncture and
no-treatment groups have been used in animal shock models.
There are many such animal studies, but animal model study
(instead of clinic study) is not used as data sources for
our articles here.
Patient in low level shock appears anxiety, cloudy
consciousness and slow reaction. Upon middle to severe
shock, patients lose consciousness. That acupuncture can
increase blood pressure when the patients is with very low
level consciousness suggests that a placebo effect is not
the only mechanism by which acupuncture works, and that
acupuncture works not only for subjective disorders, such as
pain, but also objective disorders, such as blood pressure.
9.3.
Treatment of persistent vegetative state by acupuncture
Along with the development of medical
diagnosis technique and emergency treatment, the death rate
of emergency patients has been dramatically reduced. At the
same time it also induces a new social and medical problem:
there are more patients with persistent vegetative state.
There are higher death rate and cripple rate in such group
of patients. The persistent vegetative state is hard to
treat, causes heavy burden to patient's family and society,
even if after lots of efforts of medical services. It has
become a very serious social concern in and out China.
Estraneo A
(2010)
observed 50 cases of persistent vegetative state. Under the
treatment of conventional medicine, only 10% of patients
regressed into shallow consciousness, another 14% returned
consciousness, but all happened after one year of treatment.
Before the publication of his paper, it was commonly
believed that it is almost impossible to get recovery of
consciousness for persistent vegetative state due to brain
trauma for more than one year, or due to other reasons for
more than half year.
For a long time, due to no effective way of treatment,
the attitude of medical society is negative and passive for
persistent vegetative state. In US, the doctors can stop any
treatment and nurse service to allow the patient to
euthanasia, according to patient's willingness before sick
and to the agreement of patient's family.
However, it is a quite different
picture of the treatment of
persistent vegetative state in China. A lot of studies and
clinic reports suggest that acupuncture can work to speed up
the wake-up of patients with the persistent vegetative state
(Attached list
22).
We can make a summary of these data into Fig. 23.
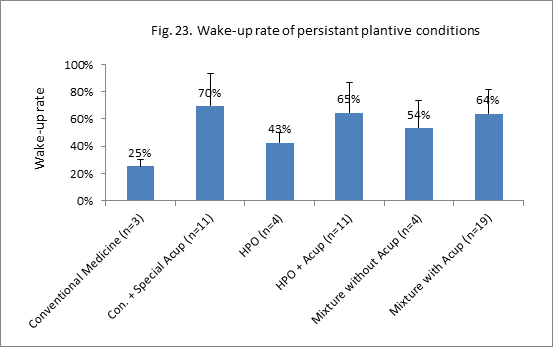
Fig. 23. n = number of experiments. Acupuncture in
the “Mixture with Acup” and “Mixture without Acup”
groups are ordinary acupuncture. Con: conventional
supportive therapies. HPO: high pressure oxygen.
Mixture: high pressure oxygen, rehabilitation therapy
(exercise), tuina, massage, physiotherapy, sound-light
simulation therapy.
Data in Fig. 23 suggest: if treated with traditional
conventional medicine, the wake-up rate for the persistent
vegetative state is 25%. Conventional medicine plus high
pressure oxygen, the wake-up rate can increase to 43%. When
the conventional medicine combined with high pressure
oxygen, rehabilitation, sound-light stimulation, it
increases furthermore to 54%. With high pressure oxygen plus
acupuncture, the wake-up rate is 67%. When high pressure
oxygen plus ordinary acupuncture, is combined with
rehabilitation, plus sound-light stimulation, the wake-up
rate remained the same (64%). Conventional medicine plus
special acupuncture, the wake-up rate reaches 70%,
suggesting that the special acupuncture technique works much
better than the ordinary acupuncture technique, and also
better than combination of complex and expensive therapies.
Even with ordinary acupuncture, its combination with high
pressure oxygen works better than combination with other
more rehabilitation remedies.
The
effectiveness
of acupuncture treatment of the persistent vegetative state
is related to the length, the severity and the cause of the
disorder, the length of treatment course of acupuncture, the
age of the patient, etc.
The longer the disorder before acupuncture treatment, the
harder the treatment. The persistent vegetative state due to
brain trauma is easier to treat than that due to
cerebrovascular accident. The persistent vegetative state
due to cerebral infarction is the most difficult to treat.
Acupuncture does not work if the length of treatment is not
long enough.
There are data
suggest that 37% to 43% of patients
with persistent vegetative state may still have slight or
shallow consciousness and be able to respond to the doctor's
order. However, such shallow consciousness is not complete
consciousness. It is similar to the consciousness in early
stage of shock, in which it can be doubted for the ability
of patient to remember things or to analyze outside
stimulation, not to speak of a hint to them. We can image
our own consciousness and ability to respond to a hint when
we did not have sleep for two nights. Yes, we have
consciousness, but our response to outside stimulation would
be very slow and our mind is cloudy to a hint. Therefore, it
would be very difficult to link the increased wake-up rate
of those patients after treatment with acupuncture to a hint
or to a placebo effect.
Here we paid attention to the wake-up rate, not to the
recovery of body function or life ability after wake up. We
emphasize that acupuncture can work when a patient is no, or
almost no, consciousness
[20].
Some paper reported not the wake-up rate, but a PVS scale.
Some reported a grade mark, such as the rate of basically
cured, dramatically cured, improved, or no change, or such
as improved, effective, no effective. For former grade
report, we choose their "basically cure + dramatically
improved" as indication of wake-up. In the later grade
paper, we only choose their "improved" as wake-up rate.
Therefore,
in the calculation of wake-up rate, we have tried to exclude
those patients who only come into a shallow consciousness
state after treatment.
9.4. Acupuncture used before or during anesthesia
梁洁
(2007)
reported the use of transcutanious electrical stimulation
(HANS machine, 30 min before anesthesia until the end of
operation, stimulating acupuncture points) for 30 cases of
breast cancer undergoing radical masectomy (HANS group). The
patients were given intravenous induction plus general
anesthesia. Another 30 similar cases were only give
intravenous induction plus general anesthesia but no
acupuncture (control group). It was found that, 12 hours
after operation, the pain level (VAS scale) in the HANS
group is dramatically less than control group (2.14±0.85 vs
3.38±0.91) . The HANS group showed much less rate of
nausea/vomit than the control group (19% vs 34%).
谢健
(2009)
treated 30 cases of patients for radical resection of colon
cancer. The patients were given general anesthesia plus
scalp acupuncture (Acupuncture group). Another 30 similar
patients were given general anesthesia only (no acupuncture,
control group). Acupuncture started 20 min before anesthesia
and lasted until the end of the operation. They found that
the involvement of scalp acupuncture reduced the pain during
skin incision (isoflurane MAC is 0.75 and 0.88,
respectively), showed some level of pain inhibit and
anesthesia (the isoflurane MAC during operation is 0.95 and
1.29, respectively). It means that the use of acupuncture
reduced the use of anesthesia drug by 26%.
欧阳铭文
(2009)
allocated
100 patients who were for Laparoscopic gastrointestinal
surgery, randomly and blindly into two anesthesia groups:
general anesthesia plus acupuncture (acupuncture group, 50
cases) and general anesthesia only (control group, 50
cases). The acupuncture (on Neiguan point both sides) was
started before induction and lasted until the end of
operation. After operation, the needle was removed. The
acupuncture points were covered with an opaque tape. It was
found that the incidence of nausea for 6 hours after the
operation was 12% and 28% in the acupuncture group and the
control group, respectively. The postoperative pain level
was no difference between the two groups
.
池浩
(2014)
randomly
allocated 160 patients who were to have heart valve
replacement operation,
into general anesthesia plus
electrical acupuncture (acupuncture group, 80 cases) and
general anesthesia only (control group, 80 cases).
Electrical acupuncture (on Zhongfu, Chize and Ximen points)
were started 20 to 30 min before induction, lasted until the
end of the operation. The anesthesia in acupuncture group
did not use trachea cannula, only
use little amount of anesthesia. The result is: the
acupuncture group and the control group had similar level of
anesthesia, but the acupuncture group showed less amount of
anesthesia drug, less case who needed blood infusion,
earlier time to get up the bed, short time to stay in
observation room, less days in hospital, less expense for
medical cost, less case with lung infection, earlier time to
start to eat, less days to use antibiotics, all of which
were significant different.
吴群
(2013)
randomly
allocated 40 cases of craniotomy into
two groups: 20 cases were given general anesthesia (control
group) and 20 cases of general anesthesia plus electrical
acupuncture (Acupuncture group). The acupuncture started 20
min before anesthesia until the end of the operation. For
the control group, electrical patch was adhered to the
acupuncture points, but no electrical was connected. They
found that, compared with the control group, the acupuncture
group showed shorter time to wake up (15 min vs 20 min)
after operation, and needed less amount of anesthesia drugs
(average 2000 mg vs 2500 mg). Note that the control group is
a sham group.
幸志强
(2012)
and his colleague randomly allocated 60 patients undergoing
subtotal thyroidectomy surgery
into two groups of anesthesia: general anesthesia group
(control group, 30 cases) and general anesthesia plus
transcutaneous acupoint electrical stimulation (
TAES)(Acupuncture group, 30 cases). TAES started 20 min
before induction of anesthesia and lasted until the end of
the operation. They found that the use of TEAS could
significantly stabolize the blood circulation (heart rate,
blood pressure), reduce the time of the extubation
(6.43±1.08 vs 10.83±2.64 min), and shorten the time to stay
in observation room (12.31±1.79 vs 17.83±2.87 min), reduced
the usage of anesthesia drugs (46.7±6.3 mg vs 67.5±5.6 mg) ,
and reduced the cost of medicine (211.78±34.5 vs
291.53±22.81 yuan).
张兆伟
(2014)
randomly and blindly allocated 60 patients undergoing
Gynecologic laparoscopic surgery into two groups: electrical
acupuncture plus general anesthesia (acupuncture group, 30
cases) and general anesthesia alone group (control group, 30
cases). Electrical acupuncture started 30 min before
induction and lasted until the end of the operation. They
observed the effect of electrical acupuncture on the gastric
function of these patients, by observing the changes of
gastric mucosal partial pressure of C02
(PgC02),
arterial partial pressure of C02
(PaC02),
and the partial pressure difference
[P(g-a)C02]
during surgery. They found that after intervention, there
were significant differences in comparing PgC02
and [P(g-a)C02]
(P<0.01, P<0.05). The intra-group differences in comparing
all indexes were statistically significant between both
groups (p<0.01). They commented that electrical acupuncture
adopted in laparascopic surgery with general anesthesia can
guarantee the supply of blood oxygen to gastric mucosa, thus
protecting the gastric function. Please note that the
control group is also a sham group.
安立新
(2011)
and
his colleagues randomly and double blindly allocated 80
patients undergoing supratentorial tumor resection into two
anesthesia groups: general anesthesia group (control group,
40 cases) and general anesthesia plus electrical acupuncture
(acupuncture group, 40 cases). The electrical acupuncture
were started from the beginning of the induction until the
end of the operation. In the control group, only attached
electric line to the acupuncture points (on skin) but no
connection to electric. Compared with the control group, the
acupuncture group showed less consumption of anesthesia
drugs, less time needed to restore automatic breath, time to
extubation, to open eyes, to restore automatic movement,
automatic direction, and shorter time to stay in operation
room. After operation, the incidence of irritation, nausea
and vomit, all were less in the acupuncture group. For
example, the time needed to open eyes in acupuncture group
and in the sham group was 18.5±8.5
min and 28.5±13.4, respectively.
安立新
(2013)
randomly
allocated 120 patients undergoing
supratentorial tumor resection into three anesthesia groups:
electrical acupuncture plus general anesthesia (acupuncture
group, 40 cases); TENS plus general anesthesia (TENS group,
40 cases) and general anesthesia only group (control group,
40 cases). Acupuncture and TENS started before induction and
lasted until the end of the operation. In the control group,
there were electrical wire attached to the acupuncture
points, but no electric connected. They found that, during
the recovery period, the time needed for automatic breath,
extubation time, time to open eyes, time to have automatic
movement, time to have direction ability, time to leave
operation room, all were shorter in the acupuncture group
and the TENS group, than that in the control group. The
postoperative pain level (VAS scale) in the acupuncture
group (3.33±1.09) and the TENS (3.40±1.30) group was lower
than that in the control group (6.43±1.52)
.
虞慧畅
(2009)
randomly
allocated 60 patients undergoing modified radical mastectomy
into two groups of anesthesia: TENS plus general anesthesia
(TENS group, 30 cases), and general anesthesia (control
group, 30 cases). TENS started before induction and lasted
until the end of operation. They found that the heart rate,
the blood pressure, blood concentration of catecholamin, and
cortisol after extubation are all increased compared that at
the end of operation in each group. The increment in the
TENS group is significantly less than that in the control
group. The Airway adverse reaction is also much less in the
TENS group than that in the control group.
宫丽荣
(2013)
randomly allocated 80 patients undergoing elder abdominal
operation into two groups: general anesthesia plus
acupuncture (acupuncture group, 40 cases) and general
anesthesia only (control group, 40 cases). The electrical
acupuncture started 20 min before induction and lasted until
the end of the operation. They found that the usage of
anesthesia drugs, the time to open eyes, the time to finish
order, and the time to restore normal direction, the
restless rate, are all lower in the acupuncture group than
those in control group. For example, the time to wake up in
the acupuncture group is 7.18±2.73
but that in the control group is 12.81±4.42 min. They
concluded that combined acupuncture assisted general
anesthesia could stabilize the hemodynamics, reduce the
stress to the surgery in elderly patients undergoing
abdominal surgery, thus being suitable and favorable for
these patients.
林舜艳
(2013)
randomly allocated
75 elderly patients undergoing colorectal cancer resection
surgery into two groups: general anesthesia plus acupuncture
(acupuncture group, 38 cases) and general anesthesia only
(control group, 37 cases). The electrical acupuncture
started 20 min before induction and lasted until the end of
the operation. They found the time needed to wake-up
was shorter in the acupuncture group than that in the
control group (20.35±6.05 min vs
28.24±7.68 min). The rate of disorder of recognition is also
low in the acupuncture group than that in the control group
(23.7% vs 35.1%).
杨琼卉
(2012)
randomly allocated
90 patients undergoing gynecologic laparoscopic surgery into
three groups: general anesthesia plus HANS (acupuncture
group I, on Zusanli and Sanyinjiao points, 30 cases) and
general anesthesia plus HANS (acupuncture group II, on Hegu
and Taizhong points, 30 cases) and general anesthesia only
(control group, 30 cases). The TENS acupuncture started 30
min before induction and lasted until the end of the
operation. They found that the Sevoflurane concentration
during operation is much less in the two acupuncture group
(acupuncture group I is much less than that in acupuncture
group II). The blood pressure and heart rate were more
stable in the acupuncture group. The time before opening
eyes and removing the tube were shorter; the anxiety
scale, pain level, nausea scale, and
incidence to hold lower jaw, are all lower, in the two
acupuncture groups than those in the control group. The time
before passing gas was also less in the two acupuncture
groups than that in the control.
周红
(2002)
randomly allocated 66 cases undergoing video assistant
thoracoscopy into two groups: acupuncture plus pain-killer
anesthesia group (acupuncture-drug group, 33 cases) and
general anesthesia group (control group).
The acupuncture started 30 min before induction and lasted until the end
of the operation. they found that the consumption of the
pain killer is much less in the acupuncture-drug group than
that in the control group (0.039±7.419 ml/kg vs 0.068±0.023
ml/kg). The blood pressure and heart rate were similar in
both group. The good anesthesia rate of the acupuncture-drug
group is 78.8%.
顾陈怿
(2004)
randomly allocated
22 patients undergoing tumorectomy into two groups: general
anesthesia plus acupuncture (acupuncture group, 11 cases)
and general anesthesia only (control group, 11 cases). The
acupuncture started 20 min before induction and lasted until
the end of the operation. They found that the inhibition
effect of the surgical operation was less in the acupuncture
group than that in the control group. The blood circulation
is more stable during the operation in the acupuncture group
than that in the control group.
顾陈怿
(2010)
randomly allocated
90 patients undergoing cholecystectomy into three groups:
general anesthesia plus traditional electrical acupuncture
(acupuncture group, 30 cases), general anesthesia plus sham
acupuncture (sham group, non-acupuncture points, also with
electric stimulation, 30 cases), and general anesthesia
only (control group, 30 cases). The acupuncture started
15-30 min before induction and lasted until the end of the
operation. The acupuncture needles in the sham group were
inserted into non-acupuncture points and also connected with
electrical stimulation. They found that the consumption of
anesthesia drug in the acupuncture group is much less than
that in the sham group and the control group. For example,
the consumption of Propofolum in the acupuncture group, the
sham and the control groups are 451.33±136.30 mg,
524.57±180.66 mg, and 600.47±153.84 mg, respectively. The
time before opening eyes, before extubation, and before
recovery of direction ability, all were shorter in the
acupuncture group, than those in the sham group and in the
control group. The use of pain killer after the operation is
also much less in the former than that in the later two
groups. The postoperative pain level was less in the former
than that in the later two groups. Acupuncture at acupoints
can enhance the anesthetic effect of compound general
anesthesia and prolong the analgesia period. Acupuncture at
non-points has certain effect , but their effectiveness is
less than that of acupoints. Thus, the acupoint has the
specificity and accurate acupoint selection is the key
factor affecting analgesia effect.
丁依红
(2013)
randomly
allocated 90 patients undergoing cholecystectomy into three
groups: general anesthesia plus traditional electrical
acupuncture (acupuncture group, 30 cases), general
anesthesia plus sham acupuncture (sham group,
non-acupuncture points, also with electric stimulation, 30
cases), and general anesthesia only (control group, 30
cases). The acupuncture started 15-30 min before induction
and lasted until the end of the operation. They found that
the acupuncture group can stabilize blood circulation,
reduce CO2
pneumoperitoneum, reduce
postoperative stress reaction, enhance postoperative
pain-reducing effect, compared with the sham and control
groups. The time before opening the eyes, time before
extubation, and time before recovery of direction ability,
all are significantly shorter than sham group and the
control group. The acupuncture groups worked better than the
sham group.
Wang You-jing (2012)
randomly
allocated 80 patients undergoing pneumonectomy into four
groups: sham group (sham acupuncture plus general
anesthesia, 20 cases), acupuncture (2 Hz) plus anesthesia (2
Hz Acupuncture group, 20 cases), acupuncture (100 Hz) plus
anesthesia (100 Hz acupuncture group, 20 cases), and 2/100
Hz acupuncture plus anesthesia (2/100 Hz acupuncture group,
20 cases). The acupuncture started
30 min before induction and lasted until the end of the
operation. In the sham group, electrical patch was attached
to the acupuncture point spots, but no electric connected.
They found that the consumption of fentanyl during
surgery is less in 2 Hz acupuncture group and 100 Hz
acupuncture group than in the sham and the 2/100 Hz
acupuncture group. In all groups, the average arterial
pressure increased after intubation, compared to that before
induction, but the increase range in all acupuncture groups
were less than that in the sham group. For similar
comparison, the heart rate increased significantly in the
sham group, but not so in all the acupuncture groups. After
the surgery, the index for auto-immune function reduced, but
not so in all the acupuncture groups. They concluded that,
with the use of acupuncture during surgery, with less amount
use of anesthesia drugs, the body circulation and immune
function can be more stable, so as to reduce body stress
reaction and to protect body important organ function. The
electrical frequency of 2 Hz and 2/100 Hz were better than
the 100 Hz.
唐育民
(2001)
randomly allocated
45 patients undergoing radical operation of carcinoma of
esophagus into three groups: electrical acupuncture group
plus general anesthesia (acupuncture group, 15 cases),
electrical patch plus anesthesia (patch on acupuncture
points, connected with electrical stimulation) (patch group,
15 cases), and general anesthesia only (control group, 15
cases).The acupuncture and the patch stimulation started
10-30 min before induction and lasted until the end of the
operation.
They observed anesthesia effect in
the tree groups. The results were: the number of patient
reached anesthesia level I in acupuncture group, patch group
and control group were 11 (73.3%), 10 (66.7%), and 4
(26.7%), respectively. The efficiency of the electrical
acupuncture plus general anesthesia, electrical patch
stimulation plus general anesthesia worked better than
general anesthesia alone. The authors commented that
acupuncture point stimulation can adjust body function
status, to increase pain threshold. Using acupuncture alone,
there is possibility that the suppression of pain is not
complete, muscle is not completely relax, and the contract
reaction is strong, so that its application in the surgical
area is limited somehow. On the other side, anesthesia drug
tends to inhibit functions of cardiovascular system and
respiratory system. Its inhibition effect is related to the
dose used. Inhibition is risk to patients with
cardiovascular diseases, if it is over used. When the
acupuncture point stimulation technique (needle or
electrical patch stimulation) is used together with general
anesthesia, the patients' heart rate and blood pressure are
stable. The patients loss consciousness without painful face
and do not realize the surgical course. The usage of the
anesthesia drug is reduced. The safety of the combined
anesthesia is increased; the anesthesia effect is remained
or improved; the cost of the anesthesia is also reduced.
付建峰
(2002)
randomly allocated 40 patients, after general anesthesia,
into two groups: TENS group (20 cases) and control group (no
TENS stimulation, 20 cases). The electrical stimulation on
acupuncture points started 10 min before skin incision, and
lasted for 30 min. They found that, the heart rate and
average arterial pressure were increased in both groups 10
min after skin incision, but the increment range in the TENS
group in much less than that in the control group. For
example, for average arterial pressure 10 min after skin
incision, it was increased by 25% and 35% in the TENS group
and in control group, respectively. Mean while, the heart
rate increased by 15.9% and 27.6%, in the two groups,
respectively. This result suggested that stimulation of
acupuncture points by electrical stimulation could stabilize
and buffer the body stress reaction due to skin incision.
Because the fact that the electrical stimulation started
after anesthesia when the patients lost consciousness, the
stabilization effect of acupuncture point stimulation cannot
be understand as any placebo effect.
郭继龙
(2002)
reported electrical stimulation of acupuncture points one
hour after general anesthesia on five patients undergoing
excision of intracranial tumor. The electrical acupuncture
could increase systolic blood pressure by
22.40±3.19 mmHg, diastolic blood
pressure by 12.00±1.41 mmHg, mean arterial pressure by
15.99±1.65 mmHg, and heart rate by 24.00±6.66 bpm. They
commented that after anesthesia, stimulation of acupuncture
can still improve cardiovascular function.
尹利华
(2005)
randomly allocated 69 patients
undergoing rectal cancer surgery into three groups:
acupuncture before anesthesia (pre-acupuncture group, 23
cases), acupuncture after anesthesia (post-acupuncture
group, 23 cases) and anesthesia alone (control group). They
found that the efficiency of anesthesia is better in
pre-acupuncture group than that in post-acupuncture group,
and much better than that in control group. Although it
cannot be excluded that this is due to the longer
stimulation of acupuncture points in the pre-acupuncture
group than in the post-acupuncture group, it indicated that
stimulation of acupuncture points after induction of
anesthesia could also enhance anesthesia level, and to
reduce the consumption of anesthesia drugs.
王庚显
(1959)
have reported long time ago the acupuncture treatment of
surgical accidents, such as stop of breath (2 cases),
diaphragmatic spasm (11 cases), tachyrhythmia (2 cases),
hypotension (2 cases) and shock (3 cases). Though the
earlier reports did not design control group, sham group,
blind group, they suggested that, under the anesthesia
condition, acupuncture can still exercise healing effects.
Such implication has been well documented in later
researchers.
Based on the reports above, it can be said that the
combination of general anesthesia with acupuncture (ordinary
acupuncture, electrical acupuncture or TENS), could
stabilize blood circulation, immune system, reduce the
consumption of anesthesia drugs, while enhance anesthesia
effect. It might be due to the reduction of the consumption
of anesthesia drugs, which makes possible shorter the
time before opening eyes, time stay in the observation
rooms, the time before extubation, the time to recover
direction ability, the lower level of postoperative
pain, and the lower incidence of postoperative nausea and
vomit.
欧阳铭文
(2009) 301
study showed that the reduction of
postoperative nausea/vomit rate is much more in the
acupuncture group than that in the sham group, suggesting
that acupuncture has its own specific healing effect.
Data from吴群
(2013),
安立新(2011),
安立新(2013),
顾陈怿(2004),
顾陈怿
(2010),
丁依红(2013),
Wang You-jing (2012)
all showed that the benefit of
acupuncture group is much higher in the acupuncture group
than in the sham group (no matter the sham is inserted or
non-inserted needles), also suggesting that acupuncture
indeed has unique healing effect in such non-conscious
patients.
Then, the question is, is the reduction in the consumption
of anesthesia drugs (and other benefit of acupuncture) due
to the acupuncture stimulation in the period before
anesthesia, or to that during anesthesia, or both? Data from付建峰
(2002) ,
郭继龙(2002)
和尹利华(2005)
indicated that even if the patients were under anesthesia
condition (without consciousness), acupuncture can still
work to stabilize blood circulation and to buffer stress
reaction of the body to surgical operation. The acupuncture
in the period before anesthesia surely would also work for
this effect,
[918-924]
and the only thing we do not know is how long such effect
could prolong into the period during anesthesia (during
operation) and after operation. A review article also
supports the positive function of acupuncture during the
anesthesia.
9.5. Acupuncture started after general anesthesia
Alizadeh R (2014)
randomly allocated 227 patients undergoin g general
anesthesia into two groups: acupuncture on Neiguan points
(112 patients) and acupuncture on Neiguan and Hegu points
(115 patients). The acupuncture started after the induction
of general anesthesia and lasted until the end of the
operation. They found that both groups can reduce the
incidences of postoperative nausea/vomit.
Arnberger M (2007)
randomly allocated 220 patients undergoing general
anesthesia into two groups: electrical acupuncture group
(110 cases) and sham group (electrical stimulation on
non-point spots, 10 cases). Both stimulation started after
general anesthesia and continued until the end of the
operation. They found that the incidence of postoperative
nausea in the acupuncture group and the sham group were 33%
and 51%, respectively, and that of vomit is 16% and 25%,
respectively.
Certainly, there was a report by
Liodden I (2015)
that acupuncture started after the induction of anesthesia
showed no more effect than a sham group. However, as pointed
out by Alraek T (2015)
that the acupuncture stimulation dose in this study was not
at all sufficient to create a healing effect in the
acupuncture group. When applied after anesthesia, the
acupuncture stimulation should be kept during the whole
course of the operation.
All of these data clearly suggested that, when the
acupuncture started after general anesthesia, in which the
patient has no consciousness, the acupuncture still works to
reduce the post-operative incidence of nausea/vomit,
suggesting that acupuncture has its own specific healing
effect, not a placebo effect. The reduced incidence of
nausea/vomit is not due to the aware of patient before
anesthesia for which group they were allocated in.
Streitberger K (2004) used
acupuncture before and after general anesthesia to patients
undergoing abdomen and breast surgical operation. They
stimulate Neiguan point for 20 min before or after induction
of general anesthesia. They found that the
post-operative incidence of
nausea/vomit in acupuncture group are
38.9%,48.1%,
while those in placebo group are 47.3% and 54.9%, suggesting
that acupuncture did not induced significant healing effect.
However, most of the acupuncture studies on this topic using
acupuncture either started before general anesthesia or
after induction of general anesthesia, and lasted until the
end of the surgical operation and the incidence of
post-operative nausea/vomit reported is between 17.7% to 21%
(see the current article). Therefore, the Streitberger
(2004) experiment does not mean that acupuncture does not
work, but that the 20-min acupuncture is not sufficient to
bring out a healing or preventive effect for post-operative
nausea/vomit.
9.6. Delayed wake-up after general anesthesia
After stop giving the general anesthesia medicine for 90
min, that the patient still does not wake-up can be regarded
as delayed wake-up. This is a common complication after
general anesthesia and one of the reasons that risk
patient's life.
翟文生
(2011)
randomly allocated 30 patients in the delayed wake-up status
into two groups: conventional medicine plus acupuncture
treatment (acupuncture group, 15 cases) and conventional
medicine only (control group, 15 cases). The acupuncture is
a kind of modified acupuncture technique. The needles were
kept for 30 min, with manipulated by hands once every 10
min. The acupuncture was repeated once every 2 hours until
the consciousness returned. In the acupuncture group, the
mean wake-up time is 150 min (30-380 min), while that in the
control group is average 300 min (90-1080 min). The
difference is significant.
张全霞
(2014)
randomly allocated 50 patients in the delayed wake-up status
into two groups: conventional medicine plus acupuncture
treatment (acupuncture group, 30 cases) and conventional
medicine only (control group, 20 cases). The acupuncture is
similar as above: the needles were kept for 30 min, with
manipulated by hands once every 10 min. The acupuncture was
repeated once every 2 hours until the consciousness
returned. The average wake-up time in the acupuncture group
is 90 min (30 min to 380 min) and in the control group, 300
min (90 min to 1080 min).
Delayed wake-up is commonly seen in elderly patients. The
reasons are varied. The old patients are with declined body
function, slower metabolic rate, and are sensitive to
anesthesia, so that it is easy to have remaining of
anesthesia drugs in the body to cause the delayed wake-up.
王春爱
(2014)
randomly allocated 80 elderly patients (after general
anesthesia and surgical operation) into two groups:
conventional medicine plus acupuncture (acupuncture group,
40 cases, acupuncture started after operation) and
conventional medicine only (control group, 40 cases). They
found that the average time before wake-up was 15.3±1.9 min
in acupuncture group, while it was 18.7±2.4 min in the
control group. The difference was significant.
9.7.
Anesthesia in shock patients
Acupuncture used in anesthesia can not only have
pain-reducing effect, but also clear anti-shock effect. When
the blood pressure of the patients are very low or no blood
pressure, it would be very dangerous to give anesthesia
drugs, since the anesthesia medicine tend to inhibit never
system, and the medicine has side effects too, both of which
could make the shock condition worse, bring risk to the
surgical operation and cause complication after the surgery.
吴蓉蓉
(1980)
treated 99 shock patients who need surgical operation. The
systolic pressure was all below 90 mmHg. The reasons for the
shock included hypovolemic shock, toxic shock, traumatic
shock, and so on. They treated the patients with
conventional medical ways, such as infusion, oxygen,
infusion of blood, antibiotics, correction of electrolyte
disturbances, and so on. Meantime, they used body
acupuncture, ear acupuncture, nose acupuncture, or mouth lip
acupuncture to the patients. After induction with
acupuncture for 15-25 min, it was observed increase in the
blood pressure. During the induction period, blood pressure
increased between 10-20 mmHg, 21-30 mmHg, 31-40 mmHg and
more than 41 mmHg were 41, 22, 7, and 14 cases. In 3 cases,
the blood pressure went down, and in 12 cases, no change.
Among the 99 cases, only 11 cases changed to epidural
anesthesia due to incomplete anesthesia with acupuncture. 15
cases needed addition of 0.5% procaine (local anesthesia
medicine). The authors pointed out that acupuncture can not
only have pain inhibition effect, but also relatively
apparent anti-shock effect. After acupuncture, 84.85% of
patients have had blood pressure increased, while at the
same time, similar patients with continuous epidural
anesthesia, no any case had blood pressure increased and 81%
of patients with blood pressure decreased, and 72% of the
patients with blood pressure down to zero. During
acupuncture, blood pressure, pulse and breath were
relatively stable (less variable). The recovery after
surgery was faster. No side effects happened. The inhibition
to respiratory system and cardiovascular system by the
anesthesia medicine was prevented.
Doctors in the department of anesthesia in the Furth
Hospital of Harbin City (1973)
reported
their treatment of 30 shock patients who needed anesthesia.
The reasons for the shock were toxic shock and hypovolemic
shock. Acupuncture was mostly body acupuncture. 12 cases
were also with auricular acupuncture. Upon skin incision, 21
cases was given little amount of local anesthesia medicine.
During surgical operation, there was no accident as
respiratory inhibition as easily seen in medicine
anesthesia. For anesthesia efficiency level, 2 cases reached
excellent level, 10 cases reached good level, 13 reached
acceptable level, and 5 cases failed and changed to medical
anesthesia. The blood pressure-increasing effect by
acupuncture is gradual with less variation. After increase,
it was easy to keep consistent, unlike the blood pressure
increased by pressor agents in which the blood pressure
could largely fluctuate. Except for 1 case whose blood
pressure did not increase, in all other 29 cases, the blood
pressure increased and kept in some level as well. The
acupuncture could work in coordination with pressor agents.
Under acupuncture, the use of pressor agents was much less
than when pressor agent alone was used; the pulse was
stronger; the difference between systolic and diastolic
pressure was larger, and breath was stronger. All of these
are helpful to solve shock condition. In hypovolemic shock,
the use of acupuncture reduced the volume of blood infusion
needed. It reduced the blood infusion average about 400 ml.
Shock patients have failure of functions of liver and
kidney. Under such condition, the use of medical anesthesia
tends to make the condition worse, especially after the
operation to cause severe consequence. Upon the acupuncture
use, no any case was with worse liver-kidney function due to
anesthesia, since the internal environment was disturbed
less with acupuncture anesthesia.
Doctors in the department of anesthesia in An-yi Affiliated
Hospital (1973)
reported the treatment of 50 cases of shock or severe
patients undergoing surgery. The shock included hypovolemic
shock, toxic shock, and traumatic shock. To the 50 cases,
used were auricular acupuncture (27 cases), auricular
acupuncture plus body acupuncture (7 cases), nose
acupuncture (6 cases), nose acupuncture plus auricular
acupuncture (4 cases), auricular acupuncture plus ear-root
point injection (1 case), auricular acupuncture plus body
acupuncture plus ear-root point injection (1 case), and nose
acupuncture plus intradermal acupuncture (4 case). After
acupuncture for about 10 to 15 min, the blood pressure could
start to increase. Together with intravenous infusion of
liquid and blood, correction of acid toxic, and pressor
agent, the blood pressure returned to normal gradually. In
all the 50 cases, blood pressure increased 10-20 mmHg, 21-30
mmHg, 31-40 mmHg, and more than 41 mmHg were 21, 16, 7, and
5 cases, respectively. Only one case was with no change in
blood pressure. The whole course of the operation was
stable. For the acupuncture anesthesia level, 43 cases are
satisfied and 7 cases were with incomplete anesthesia and
had changed the way of anesthesia. Among the 43 success
cases, 8 cases used local anesthesia in the skin incision
spot with 0.5% procaine.
It was commented
that the adrenal gland point on ear has stronger
blood pressure-increasing effect. Nose acupuncture works
better for surgical operation in lower abdomen for loss
muscle. Nose acupuncture plus intradermal acupuncture works
satisfied for reducing pain during skin incision. Using
acupuncture in hypovolemic shock, the volume of blood to
infusion can be reduced but the blood pressure goes up
gradually. It was commonly found that, with medical
anesthesia, the increased blood pressure can reduce again,
so that the use of pressor agents is very common. But it
would be dangerous to use large amount of pressor agents.
With acupuncture for anesthesia, it is rare that the blood
pressure would go down again. The author[1]
reported that they treated 50 cases of shock or severe
patients, except for only one case, other patients had blood
pressure increased after acupuncture induction. Only 12 out
of the 50 cases used little amount of pressor agents, which
was much less than with ordinary medical anesthesia.
Therefore, acupuncture used in shock patients also prevented
the side effect of pressure agents (especially as
noradrenalin), such as skin necrosis and reduced volume of
urine. With intratracheal anesthesia, the chance of
complications increased, but with acupuncture anesthesia, it
was never seen such complication as respiratory inhibition
as seen with former.
Doctors in the department of anesthesia in Affiliated
Hospital of Shandong Medical College
(1973)
reported their treatment of 45 shock patients undergoing
anesthesia. Among the 45 cases, light shock, middle shock
and severe shock were 8, 26, and 12 cases, respectively.
Most of patients did not get any medicine before
acupuncture. Several patients got pain killer Sauteralgyl,
or sedative Phenergan, or atropine or Dong Lang scopolamine.
Among the 45 cases, 33 cases combined with local anesthesia
(73.3%); 27 cases with Sauteralgyl (60%). 12 cases did not
use any of these medicine (26.7%). The anesthesia
efficiency: very good is 71.1%, not good is 28.9%. Blood
pressure increased in 82.2% of patients; not changed in
6.7%; reduced in 11.1% of patients, at the end of the
surgical operation.
Doctors in the anesthesia group of the Fifth People's
Hospital of Guangzhou City
(1975)
reported their treatment of 55 shock patients who needed
surgical operation. The operation included cesarean,
subtotal gastrectomy, ectopic pregnancy, ovariocystectomy,
cholecystectomy, intestinal resection and anastomosis,
splenectomy, debridement and suture fixation. Before
operation, used was only sedative luminal. Before and during
the operation, used only the acupuncture for anesthesia (did
not use anesthesia). The anesthesia efficiency: very good
level is 67.3% of patients; more than 100 mg of
Sauteralgyl was needed in another
25.4% of patients. Acupuncture anesthesia failed in 7.3% of
patients. Postoperative blood pressure increased more than
100 mmHg in 87.2% of patients; increased 80-90 mmHg in 10.9%
of patients and failed to increase in 1.8% of patients. Only
in 2 cases needed pressor agents.
杨生泰
(1987)
reported their treatment of 60 shock patients undergoing
anesthesia and surgical operation. Among the 60 cases, 28
were hypovolemic shock and 32 infectious shock.14 cases used
50 mg Sauteralgyl, 0.5 mg
atropine. 16 cased used 50 mg Sauteralgyl only. 7 cased used
0.5 mg atropine only. They did not use any other pain killer
or sedative. 56 cases used auricular acupuncture, and 4
cases used body acupuncture. The anesthesia efficiency:
reached level I, II, III, and IV were 21, 22, 12, and 5
cases, respectively. The authors stated that for abdomen
surgery, auricular acupuncture worked better.
Doctors in the acupuncture anesthesia group in the Shanggao
County People's Hospital of Jiangxi Province
(1977)
reported their treatment of 37 shock
patients who needed surgical operation. They used
acupuncture to 37 patients (acupuncture group), and medical
anesthesia (medical anesthesia group) to 15 cases (including
general anesthesia, lumbar anesthesia, Epidural anesthesia,
and local anesthesia). In the acupuncture group, most of the
patients did not use sedative, little patients used pain
killer 25-50 mg Sauteralgyl and used local anesthesia during
operation. The shock was mostly hypovolemic shock and toxic
shock. In the 37 patients, blood pressure increased after
acupuncture was 70.3%; no change was 24.3%; reduced was
2.7%; and fluctuated was 2.7%. In the medical group, the
blood pressure increased in 13.3%; not changed in 26.7%;
reduced in 40% and fluctuated in 20% of patients. Anesthesia
efficiency reached level I, II, and III in the acupuncture
group was 29.7%, 56.8%, and 13.5%, respectively.
The Acupuncture-anesthesia cooperation group in Yuling,
Guangxi Province
(1977)
reported acupuncture anesthesia to 88 shock patients who
needed surgical operation. The shock was hypovolemic and
toxic shock. The surgery was stomach, intestine, gall
bladder, and uterine surgery. During acupuncture and
operation, blood pressure increased less than 10 mmHg was 39
cases; increased 11 - 20 mmHg was 10 cases; increased 21-30
mmHg was 7 cases and no change was 32 cases.
胡宗泽
(1978)
reported acupuncture anesthesia to 60 shock patients who
needed surgical operation. Among the patients, 26 were
hypovolemic shock; 28 were toxic shock; and 6 were traumatic
shock. 30 min before the operation, patients were given 0.5
mg atropine, 0.1 g luminal sodium intramuscular injection.
The acupuncture anesthesia was: nose acupuncture plus
auricular acupuncture 49 cases; nose acupuncture plus
auricular acupuncture plus body acupuncture 8 cases. Before
operation, Sauteralgyl was injected intramuscularly. It was
not used if the condition was not severe. The anesthesia
efficiency reached level I, II, III, and IV, was 10, 19, 29,
and 2 cases, respectively. After acupuncture started,
intravenous infusion of liquid and blood, and oxygen
inhalation, and others were started too. After 15-20 min of
acupuncture, blood pressure started to increase. At the end
of operation, 91.6% of patients had blood pressure increased
gradually with larger difference between the systolic and
diastolic pressure. The heart beat sound stronger gradually
and the microcirculation started to be improved gradually
too. In the 32 patients with hypovolemic and traumatic
shock, the systolic pressure increased average 24 mmHg, in
which 12 patients increased 30 mmHg. In the 26 hypovolemic
shock, the hemochrome was average 7.6 g, average loss of
blood 1500-1800 ml, while the blood infusion needed was only
230 ml, which was less than 1/6 of the lost blood volume.
Doctors in the People's Hospital of Guangxi Province
(1975)
reported
acupuncture use to 61 shock patients who needed surgical
operation. The reasons of the shock were hypovolemic (14
cases), toxic (19 cases), traumatic (2 cases), and severe
diseases (26 cases). The acupuncture included: body
acupuncture 27 cases; body acupuncture plus auricular
acupuncture 15 cases; body acupuncture plus mouth lip
acupuncture 4 cases, body acupuncture plus nose acupuncture
5 cases, auricular acupuncture 2 cases, mouth lip
acupuncture 5 cases, and no record 3 cases. The anesthesia
efficiency was excellent 55.7%, accepted 37.7%, and failed
6.5%.
For the use of acupuncture to shock patients, as summarized
by doctors in the department of anesthesia in the Affiliated
Hospital of Shandong Medical College
(1973): (1),
acupuncture could clearly increase blood pressure. The most
safe anesthesia in shock patients is local anesthesia but it
was found that when the operation area is too large, the
local anesthesia is hard to produce complete anesthesia and
satisfied relax of muscle. During the operation, blood
pressure could reduce due to the operation stimulation, the
pain reaction, and the pulse could become faster, so as to
make the shock worse, even cause accident death. In the
intravertebral anesthesia, it is inhibited the use of
intraspinal anesthesia in the shock patients. The epidural
anesthesia is neither good choice for shock patients.
Because the shock patients had poor tolerance to the
medicine used in
epidural anesthesia, personal variation is very large, it is
very easy to cause relative over-dose of anesthesia due to
improper anesthesia, so as to cause blood pressure reduced
to accident die. Ether inhalation is hard to keep stable and
even shallow anesthesia and the breath tract is hard to keep
smoothly open. It is also not good choice for a shock
patient and it should be prevented to use in shock patient.
The most ideal anesthesia might be the combination of ether
and muscle relaxer. It can not only induce satisfied muscle
relax and keep opening breath tract, but also reduce the use
of ether and keep longer time and evenly shallow anesthesia;
block the operation stimulation to the brain, to provide
satisfied muscle relax and keep open the breach tract.
However, this way of anesthesia need expert skill of the
anesthesia operator and the equipment is complex. The
advantage of acupuncture used in the shock patients is (1),
it does not use medicine, so no possibility to inhibit
respiratory or blood circulation system, so not interfere
the body function. (2), acupuncture per se has no side
effect, but has benefit to the body function (as to
stabilize body internal environment). (3), for acute
patients, especially for acute traumatic upper digestive
tract bleeding, acute intestine obstruction, there is no way
to inhibit food intake to empty stomach. Because during the
acupuncture, the patients are awake, so prevented the chance
of vomit or mis-inhalation accident. (4), acupuncture to
shock patients, the anesthesia efficiency is satisfied, and
it is simple to operate. The most realization with the
acupuncture anesthesia is safe and ensured no worry about
possible overdose of medicine or block of breath tract, etc.
Therefore, it is easy to be handled by ordinary anesthesia
operators, and it is a better choice for shock patient
undergoing surgical operation.
From above reports, it can be seen that, acupuncture alone
can be used in shock patients, to reduce the amount of usage
of pain killer and sedative medicine, the volume of blood
infusion, to reach satisfied anesthesia level and to improve
shock condition the same time.
Because the shock patients are in severe diseased condition,
their consciousness are cloudy, or even lost, they are hard
to react to outside language or action hint to cause a
placebo effect.
Someone may have questioned that for the acupuncture
anesthesia, there is still the use of pain killer and
sedative medicine. The above data showed that for most
patients and in most reports, the pain killer and sedative
are not used. Even they are used, the amount are in a level,
in which it cannot normally produce satisfied anesthesia
effect by them.
9.8.
Dementia treatment by acupuncture
Dementia can be separated at least into senile dementia and
vascular dementia. Vascular dementia is one of the common
kinds of dementia in China, which is caused by disorder in
brain blood circulation. The word dementia describes a set
of symptoms that can include memory loss and difficulties
with thinking, problem-solving or language. In vascular
dementia, these symptoms occur when the brain is damaged
because of problems with the supply of blood to the brain.
It has become a serious problem to human mental health, and
has caused a severe burden to the family life and society
too. It is a hard task for medical society to solve. It was
reported that among patients over 65 years of age, about one
third (25% - 41%) would develop into vascular dementia
within three months after acute cerebral accident.
Epidemiologic study in US showed that among survivors over
60 years of age from acute cerebral accident, about 26.3%
developed vascular dementia.
951
Currently, there is no effective therapy for the treatment
of any kind of dementia.
Because dementia patients have slow mental reaction,
analysis, and poor memory, it would be hard to believe that
those patients can react to a hint, as normal people, to
develop a placebo effect during treatment. So, let us have a
look at how acupuncture can work for dementia.
Data in Attached list
23a,
23b,
23c
are collected from China.
As usual, the effective rate from China was either reported
as grade improvement (cure, much improved, improved, or no
effect), or as MMSE scale (or HDS scale) change. For the
grade reports, we combined the "cure rate" and "much
improved rate" together and got Fig. 24a. For the later, we
got Fig. 24b.
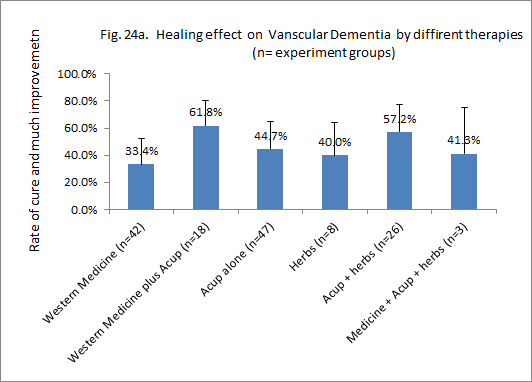
Fig. 24a. n = experiment
groups.
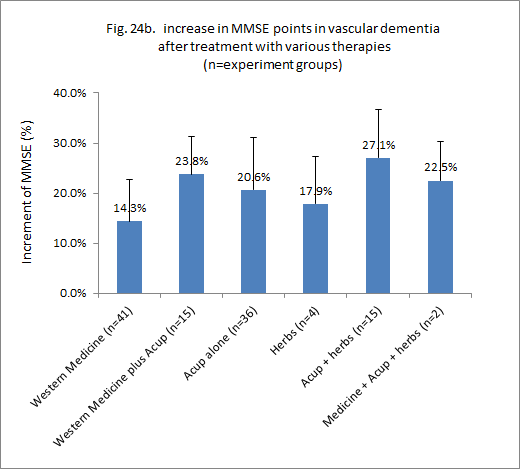
Fig. 24b. n = experiment groups.
Data showed as MMSE change (Fig. 24b) also showed
similar results
[22].
The effective rate of acupuncture group (20.6%±11%)
is higher than conventional medicine alone (14.3%±8%).
With the combination of conventional medicine with
acupuncture, the MMSE scale increased by 23.8%±8%. With
the combination of acupuncture with Chinese herbal
therapy, MMSE can be increased by 27.1%±10%.
When the healing effect is expressed with the HDS scale, the
results were similar (Fig. 24c).
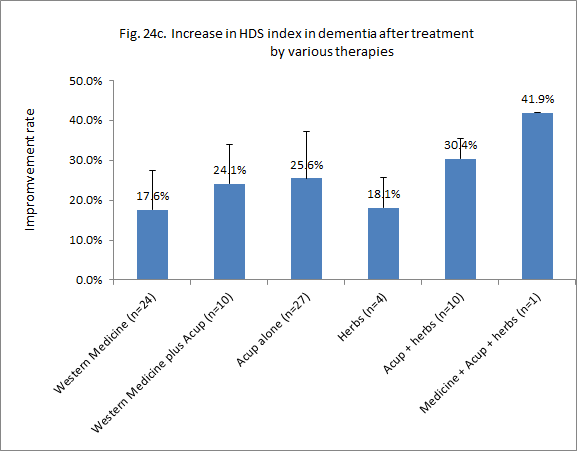
Fig. 24c. n = experiment groups.
Apparently, acupuncture has its one specific healing effect.
Combination of acupuncture with either conventional medicine
or Chinese herbal therapy can further increase the healing
effect.
Fig. 24a showed that, treated with conventional medicine,
the Cure-much-improved rate is
33.4%±19%.
With the treatment with acupuncture, it was 44.7%±20%. With
Chinese herbal therapy, it was 40.0%±24%. With combination
of conventional medicine and acupuncture, it was increased
to 61.8%±19%. With combination of acupuncture and Chinese
herbal therapy, it is similarly increased to 57.2%±20%.
9.9. Anesthesia by acupuncture alone or combined with local
anesthesia
Acupuncture can
not only work during general anesthesia to reduce the
consumption of anesthesia drugs, enhance anesthesia effect,
and reduce the post-operative side effect of surgical
operation, but also work alone or together with nerve
blocking anesthesia or local anesthesia to enhance the
anesthesia effect and reduce side effect of the anesthesia
drugs
It has been
reported in earlier years
that, when acupuncture alone was used in 138 patients
undergoing nose surgical operation, the anesthesia
efficiency reached level I was 39 cases (28.2%), level II 72
cases (52.1%). Most of the operation is correction of nasal
septum (58 cases) and nasal polypectomy (42 cases). The
patients were given 0.06 g of phenobarbital (sedative drugs)
before going to bed the day before the operation, and again
the same dose one hour before the surgical operation. Only
in 28 cases (20.2%), it was used pain killer Sauteralgyl.
Another clinic
report
stated that to use acupuncture alone for local anesthesia to
254 patients undergoing nose surgical operation (did not use
electrical stimulation), the anesthesia level reached level
I, II were 203 cases (79.9%) and 30 cases (11.8%),
respectively. They did not report whether the patients
were given any sedative drugs.
周继福 (1989)
summarized
their use of electrical acupuncture anesthesia to patients
undergoing ear-nose-through surgical operation. Among their
2046 patients, the anesthesia efficiency level reached level
I and II are 90.2%. They did not mention if their patients
were given sedative or not before acupuncture. The author
stated that the anesthesia efficiency and the acupuncture
stimulating dose had close relationship. The anesthesia
efficiency (especially muscle relax) and pain reduction
effect under longer time acupuncture induction (30-60 min)
is better than short time induction (less than 30 min).
Acupuncture anesthesia not only stimulates clear pain
reduction and muscle relaxation effect, but also works to
modulate or adjust functions of various organs and has some
other biophysiological effects. To perform endoscopic
examination under mucosal surface anesthesia, the patients
usually feel palpitation, short of breath, difficulty
feeling in chest, etc. This phenomenon was never observed
during acupuncture anesthesia.
孙鎏熙 (2001)
randomly
allocated 96 patients undergoing nasal polypectomy into two
anesthesia groups: electrical acupuncture anesthesia
(acupuncture group, 50 cases) and local anesthesia alone
(control group, 46 cases). The anesthesia efficiency: 100%.
In the acupuncture group, the surgical operation was
finished without use of any complementary medicine in 46
cases. Only 4 cases were given 10 mg diazepam or 50 mg
pethidine. The anesthesia efficiency reached level
excellent, good, and no effect, was 92%, 8%, and 0%, while
those number in the control group was 60%, 40%, and 0%.
张道武
(2002)
randomly
allocated 60 patients undergoing
nasal polypectomy into two anesthesia groups:
acupuncture anesthesia (acupuncture group, 30 cases) and
local anesthesia (control group, 30 cases). In the
acupuncture group, 36.7% of the operation reached local
anesthesia level I with acupuncture alone. In 63.3% of
cases, it was added with local anesthesia drugs, but the
amount of the drugs were less than used with typical local
anesthesia group. The incidence of postoperative pain was
less in the acupuncture group than in the control group.
童秋瑜
(2012)
randomly allocated 60
patients undergoing nasal endoscopy
into two anesthesia groups: acupuncture plus amethocaine
anesthesia (combined group, 30 cases) and amethocaine
anesthesia (control group, 30 cases). In the combined group,
the usage of amethocaine is 71.33±8.90 mg, while that in the
control group, 118.33±26.21 mg. Pain level was lower than in
the combined group than in the control group, and the
satisfied rate was higher in the former than in the latter
group.
It has been reported
that 80% patients had stress; some had depression or fear,
before surgical operation. Some patients undergoing local
anesthesia showed anxiety or shock, or changes in heart rate
and blood pressure, etc., due to too heavy emotional stress.
There are rich nerves in the nose-throat area and it is very
tender to pain in this area. The way of local anesthesia in
this area is mostly surface anesthesia or local infiltration
anesthesia.354
Some researchers
had a survey to 100 patients undergoing nasal surgery under
local anesthesia and found that 32 patients showed heavy
sweat, anxiety, nausea, palpitation, short of breath, fast
pulse, change in heart rate and blood pressure, etc.,
affecting the continuing of the operation. Apparently local
anesthesia cannot reach satisfied anesthesia effect. The use
of general anesthesia is used in the nasal endoscopic
surgery can avoid the incomplete anesthesia (as by local
anesthesia), so to ensure the continuing and finish of the
surgery operation. However, it needs trachea cannula to help
keep smooth breath. Because the trachea cannula is close to
the operation area, it can cause difficulty for the
manipulation of operation. Also due to trauma and
stimulation to the throat, it is easy to cause bleeding and
swelling. There is rich nerves and blood in the face, mouth,
and jaw, it is easy to cause bleeding, so to cause block of
breath tract after general anesthesia .
After nasal endoscopic surgery, it
is needed to fill the nose cavity; the patient has to
breathe by mouth. If the throat has swelling or other
trauma, the postoperative reaction would be very strong.
Therefore, the general anesthesia is neither a perfect way
of anesthesia in nasal surgery, though it can create
complete no pain status. The data above suggests that,
acupuncture anesthesia can dramatically reduce the dosage of
anesthesia medicine during the surgical operation. The
combination of acupuncture with local anesthesia medicine
used less amount of the local anesthesia medicine, so
reduced the chance of swelling of local tissue, while the
pain reduction level is still satisfied. Apparently, the
combination of acupuncture and local anesthesia medicine
could reduce the side effect and weakness of the local
anesthesia and improve the quality of surgical operation.
雷健
(2000)
and his colleagues randomly allocated
532 patients undergoing thyroid operation into two
anesthesia groups: acupuncture anesthesia group (acupuncture
group, 324 cases, with sedative before acupuncture) and
Superficial cervical plexus block anesthesia (control group,
208 cases). It is reported that the usage of meperidine in
the control group is more than that in the acupuncture
group. There was no difference for the average arterial
pressure and heart rate in each stage of the operation
between the two groups. There were no complications in the
acupuncture group, while there were 12 cases of recurrent
laryngeal nerve paralyses and 6 cases of diaphragmatic
paralysis in the control group.
马越英
(2005)
randomly allocated 100 patients
undergoing thyroid operation into
three anesthesia groups: electrical acupuncture anesthesia
(acupuncture group, 20 cases), cervical plexus block
anesthesia (plexus group, 40 cases) and the combined
acupuncture and cervical plexus block anesthesia (combined
group, 40 cases). They found that the heart rate and blood
pressure in the acupuncture group and the combined group was
more stable than that in the plexus group. There are no
recurrent laryngeal nerve paralyses or diaphragmatic
paralysis in the acupuncture group. There are 3 patients
with recurrent laryngeal nerve paralyses and 1 diaphragmatic
paralysis in the plexus group. There is 1 patient with
recurrent laryngeal nerve paralyses and no diaphragmatic
paralysis in the combined group.
There are also large amount of other studies
, reported that with acupuncture anesthesia in the thyroid
surgical operation, the vital sign is stable and there is no
side effect as those caused by medical anesthesia drugs. The
complication is little, so favoring the recovery of
patients after the operation. However, upon handling the
upper part of the thyroid or separating the tissues around
the trachea, most of patients showed more or less tractive
reaction, suggesting that the acupuncture anesthesia is not
a complete anesthesia yet. cervical plexum anesthesia does
not affect the breath of patients; the anesthesia efficiency
is ensured; and is simple to manipulate. So it is wildly
used in the surgical operation of neck area. However, after
cervical plexum block, the heart rate and blood pressure
increase, so that the heart consumption of oxygen also
increases, which is not good for patients with
hyperthyroidism, hypertension and coronary heart disease.
The combination of acupuncture with cervical plexum block
anesthesia, the pain reduction was enhanced and the usage of
the drugs was reduced about 40%-50%
,
so also prevented increase in the heart rate and blood
pressure caused by cervical plexum block anesthesia alone.
高成杰
(2004)
randomly allocated 60 patients undergoing appendectomy into
two anesthesia groups: acupuncture plus epidural anesthesia
(combined group, 20 cases), and sauteralgyl alone
(sauteralgyl group, 20 cases) and epidural anesthesia alone
(epidural group, 20 cases). Their results were that the pain
reduction effect of the combined group was much better than
the other two groups. The pain reduction excellent rate was
100%, 85%, and 70% in the combined group, the
sauteralgyl group, and the
epidural group, respectively. In the combined group, the
heart rate, blood pressure, mean arterial pressure, all were
stable, but those parameters in the other two groups,
increased. .
吴焕淦
(2007)
summarized the experience of doctors in their hospital
(1960-1987) about the use of acupuncture anesthesia in
lobectomia pulmonalis. The skin incision was 24-27 cm long.
The process of the surgical operation included skin
incision, muscle incision, strip of bone membrane, cutting
of rib, open of chest, separation of adherence, clearing of
sick tissues, clearing of blood vessels, separation of space
of lobs, prevention of mediastinal flutter, prevention of
cough, close of chest, sew of muscle, sew of skin, insert of
drainage-tube and so on for 15 steps. Acupuncture was used
mostly to reduce pain when the operation touched the skin,
muscle, and bone, and to control the fluttering of
mediastinal. In this early stage,
they used mostly manual acupuncture for anesthesia. The
patients were completely clear in mind. No tubulation used,
no medicine used and very rarely used local anesthesia
drugs. They finished totally 1385 cases. The excellent
anesthesia rate was 65.12%. In later stage, they studied the
use of acupuncture plus general anesthesia in 1089 patients
for lobectomia pulmonalis. They found that by this
combination, the dosage of anesthesia drug was reduced by
42%-45%, compared with the medical anesthesia alone. With
intramuscular injection of weak opioid analgesic drugs
Tramadol 100 mg and acupuncture-effective enhancing cerucal
20 mg, the dose of the medical anesthesia can be further
reduced by 45%, while the pain reduction effect was further
improved. The combined anesthesia can not only reduce
cardiovascular reaction during trachea cannula and tracheal
extubation during induction of general anesthesia, but also
reduce the total amount of the use of the anesthesia drugs,
so as to make the blood circulation more stable and the
wake-up earlier after the operation. From year 2001 till
now, they turned to study the influence of acupuncture on
the immune system in lung cancer patients undergoing
surgical operation. They have finished the combined
acupuncture and general anesthesia 898 cases. The dosage of
the general anesthesia in the combined group is the same as
that used in the general anesthesia group alone. They found
that acupuncture can not only work to reduce pain, but also
has immune adjusting effect, so as to improve the healing to
the lung cancer, to be benefit to the recovery of such
patients after surgical operation. They found that the
acupuncture anesthesia can increase the number of the
subgroup of T8 lymph cells at the 8th day after operation,
increase the number of the subgroup of T3 lymph cells on the
forth chemotherapy, increase the activity of NK cells, and
increase the serum γ-interferon, so to increase the immune
function of the cancer patients.
吴玉芳
(2002)
randomly allocated 40 patients undergoing colonoscopy into
two anesthesia groups: acupuncture anesthesia (acupuncture
group, 20 cases), and general anesthesia (control group, 20
cases). They found that acupuncture induced better pain
deduction.
When acupuncture was used alone or combined
with various local anesthesia methods, the patients are
clear in mind. So, those of people who insist that
acupuncture is only a placebo effect would again say that
the effect of acupuncture in the local anesthesia is also a
placebo effect. We do not deny that there could be some
placebo effect that could contribute to the good anesthesia
effect in the acupuncture group, but it appears hard to set
up a sham acupuncture group to test this hypothesis. Can we
hint the patient that he will have acupuncture which could
reduce his pain to zero during the operation, and we do a
sham acupuncture (pseudo-acupuncture, such as just put a
patch on the skin but no any electrical stimulation
connected to the patch), pretend that we are perform an
acupuncture to him, and then to cut a 24-27 cm open on the
skin of the patient? Who had ever and who dare to study sham
acupuncture as such? Remember that even in a sham surgical
operation, the researchers used local anesthesia before they
cut the skin and then sewed the cut, to pretend that a
surgical operation was done! That is a sham surgical
operation, in which the operation per se was not performed.
But here, it means a sham anesthesia, the anesthesia was not
given, but the patient would get the skin cut.
Surely in some studies, there was a use of sedative before
the acupuncture. Colquhoun D
mentioned this, and hinted that acupuncture per se does not
work but the sedative. This is a misleading to the public.
Sedative can work to calm down anxiety but not to reduce the
pain level. Also, the sedative can also produce some placebo
effect. Can anyone only use sedative (even little amount of
pain killer, such as Sauteralgyl 50-100 mg) to start a
surgical operation? Why you dare not to use the placebo
effect from the sedative and pain killer as such, but dare
to use the placebo of acupuncture to finish the surgical
operation?
Because it is hard to design a sham group in the
acupuncture-induced local anesthesia study, we indicated
that the data here is indirect evidence that acupuncture is
not a placebo effect. We can only prove our opinion by the
effect of acupuncture used before, during, or after a
surgical operation (above), in which the patients were
without consciousness but acupuncture still worked. If we
accept the conclusion from these previous studies with
general anesthesia, we should now comment that, even if
there could be some level of placebo effect in the
acupuncture-induced local anesthesia, acupuncture still
exercises its unique anesthesia effect.
Brief summary:
(1). Placebo effect needs that the person is in a clear mind
condition. Data here showed that acupuncture works in a
condition when a person is without or with very week level
of consciousness, such as coma, shock, persistent vegetative
state, general anesthesia (before, during, of after
operation). This is direct evidence that acupuncture has its
own specific healing effect.
(2). Data in the acupuncture treatment of dementia and in
local anesthesia are listed as indirect evidence, since in
the dementia, low level of patient could still have clear
mind though they could have less ability to remember; in the
local anesthesia, there is no sham data allowing a direct
comparison between the acupuncture group and the sham group.
Chapter 10. Different healing effect with different
acupuncture technique
If acupuncture is only a placebo effect, then under the same
experiment conditions, acupuncture on different acupuncture
points, or manipulate the needle by different ways, or use
different frequency of electrical stimulation... should
yield a statistically similar or the same results. Indeed,
there are some studies by acupuncturists in the Western
countries on this topic, which showing so. However, when we
review these studies, we again found that they performed
acupuncture in a quite low treatment frequency, while
similar studies by acupuncturists in China were performed in
higher treatment frequency, and found quite different
results, suggesting that acupuncture points have relative
specificity, and that acupuncture is not a placebo effect.
10.1. Different acupuncture points
于慧娟
(2014)
randomly and single-blindly allocated 50 patients with
cardiac premature beat into two acupuncture groups:
electrical acupuncture on Neiguan points (Neiguan group, 30
cases) and on Xuanzhong points (Xuanzhong group, 20 cases).
They found that the total effective rate in the Neiguan
group is 50%, while that in the Xuanzhong group, 5%. They
did the acupuncture once a day for 10 days.
许凯声
(2014)
randomly
allocated 82 coma patients due to severe traumatic
craniocerebral injury into two groups: acupuncture on
Suliao-focused point (Suliao group, 42 cases) and on
Shuigou-focued point (Shuigou group, 40 cases). Under the
same way of acupuncture, the cure-improve rate in the Suliao
group is 45.2%, while that in the Shigou point is 22.5%. The
acupuncture was performed once a day, five-day a week,
two-week as a course.
Yiu E (2004)
randomly allocated 24 dysphonias patients into two
electrical acupuncture treatment groups: acupuncture on
Renyin, Lieque and Zhaohai points (12 cases) and on Kunlong
and Houxi points (control, 12 cases). The acupuncture was 10
sessions within 20 days. After treatment, the voice
frequency range in the former increased by 28.8%, while
almost no change in the control group.
Yu YP (2010)
randomly allocated 66 cases of
primary dysmenorrhea women into two acupuncture treatment
groups: acupuncture on Sanyinjiao (33 cases) and on
Xuanzhong points (33 cases). The acupuncture was performed
during the menstruation for 5 min. They found that, the
deduction in the pain level and the increase in the arterial
blood flow in the Sanyinjiao group was much dramatic than
that in the Xuanzhong group.
|
岑珏
(2007)
randomly allocated 138 patients with unstable urine
bladder function into two acupuncture treatment
groups: acupuncture on Huiyang points (93 cases) and
on Huantiao point (45 cases). After three times of
acupuncture, various symptoms in the Huiyang group
were significantly improved, while only urine
retention feeling and urgent feeling were improved
in the Huangqtiao group. Both groups could reduce
I-PSS scale and to improve
quality of life but the Huiyang group worked better
than the Huantiao group. After 5 times of
acupuncture, the healing effect was even better than
that for acupuncture for 3 times in the Huiyang
group. They commented that, acupuncture on Huiyang
points could adjust the function of urine bladder
and the effect can be accumulated with more times of
acupuncture treatment.
|
|
赖新生
(2006)
randomly allocated 50 VD patients into five
electrical acupuncture groups: conventional
acupuncture group (Convention group); conventional
acupuncture plus Baihui points (Baihui group); plus
Shuigou point (Shuigou group); plus Shenmen points
(Shenmen group), or plus Baihui, Shuigoud and
Shenmen points (combined group). Each group was 10
patients. The acupuncture was performed once a day
for 5 days, had a break for 2 days. Repeated this
way for 6 courses. They found that after treatment,
the SECF sore in the combined group was dramatically
increased. In the Baihui group, the ability of
direction, short term memory, long term memory,
animal name memory, calculation, classification and
category separation, etc. improved dramatically. In
the Suigou group, the ability of direction, money
spending, calculation, classification, and grouping
were much improved. In the Shenmen group, the range
of figure, name of animals, classification
and grouping were much improved. They summarized
that the acupuncture points Baihui, Shuigou, and
Shenmen could improve the recognition of VD
patients. There was relative specificity of their
healing effects. The combination of the tree points
worked better than use them individually.
余明哲
(2001)
randomly allocated 64
patients with duodenal ulcer into 4 acupuncture
treatment groups: point Zusanli plus ranitidine
(Zusanli group, 16 cases), point Shangjuxu plus
ranitidine (Shangjuxu group, 16 cases), point
Xiajuxu ranitidine (Xiajuxu group 17 cases), and
ranitidine alone group (15 cases). They found that
the three acupuncture groups worked better than the
ranitidine group in the improvement of
pain-cessation time, clear rate of Helicobacter
pylori and some other symptoms. Again the Zusanli
group worked better than the Shangjuxu group and
Xiajuxu group. But the Shangjuxu group and the
Xiajuxu group worked similar. They commented that
acupuncture worked in the treatment of duodenal
ulcer using the Zusanli, Shangjuxu and Xiajuxu
points, but there was relative specificity in the
extent of healing effect among the three points.
王德军
(2012)
randomly allocated 116 functional indigestion
patients into three acupuncture treatment groups:
acupuncture on Zuyangming stomach meridian points
(point group, 36 cases), on other points on the same
meridian but they are normally not used for the
treatment of indigestion (non-points group, 39
cases), and on spots that does not belong to any
acupuncture points or meridians
(non-meridian-non-points group, 41 cases, shallow
insertion). Acupuncture was performed once a day for
five days, with a break of 2 days before next
healing course. Totally 4 courses. After the
treatment, the improvement in FDI score and SF-36
scour in the point group was much better than that
in the other two groups. The improvement of these
two parameters in non-points was also better than
that in the non-point-non-meridian points.
Apparently there are relative specificity among
acupuncture points and between the acupuncture
points and sham points.
兰蕾
(2010)
randomly allocated 60 patients who suffered from
functional indigestion, into two acupuncture
treatment groups: acupuncture on specific
acupuncture points that are normally used for the
treatment of indigestion (acupuncture group, 30
cases) and acupuncture on non-points. The
acupuncture was performed once a day for 5 times,
and continued for 4 courses. They found that, after
the treatment, the improvement of symptoms of upper
stomach bloating feeling, early fullness, upper
stomach pain and upper stomach burning sensation,
were 85.72%、78.26%、94.11%、60%
in the acupuncture group, while they were 19.23%、20%、6.25%、7.69%,
in the non-point groups, respectively. Though the
non-point stimulation also showed some improvement
compared with before-acupuncture, but the
improvement in the acupuncture group always much
better than the non-point group.
马婷婷
(2015)
randomly allocated 230 patients with functional
indigestion into two acupuncture groups: acupuncture
on far-away points (far-away group, 116 cases) and
acupuncture on local points (local group, 114
cases). The acupuncture was once a day for 5 days,
total 4 weeks. After treatment, the healing effects
of the far-away group were much better than the
local group.
何希俊
(2006)
randomly allocated 278 peripheral facial palsy
patients into two acupuncture groups: acupuncture
on far-away points (far-away group, 145 cases) and
acupuncture on local points (local group, 133
cases). The acupuncture was once a day for 6 days
per week, total 3 weeks. After treatment, the
healing effects of the far-away group were much
better than the local group. The
cure-much-improvement rate in the far-away group was
88.3%, while that in the local group, 64.7%.
We noticed that
acupuncturists in the Western countries also did
some comparison studies to test if there is
difference in the healing effect between different
acupuncture points, or between acupuncture points
and non-points. For example,
Allen JJ (2006)
randomly allocated 105 severe depression patients
into 3 acupuncture treatment groups: acupuncture on
traditional acupuncture points that are normally
used for the treatment of depression (acupuncture
group, 53 cases), and acupuncture on non-specific
points that are normally not used for the treatment
of depression (non-specific group, 52 cases), and
that on non-points that do not belong to any
acupuncture point/meridian (non-points group, 52
cases).
The acupuncture was performed twice a week for 4
weeks, than once a week for another 4 weeks (typical
Western style acupuncture). After the
treatment, the improvement rates in the three groups
were 43.5%, 47.8% and
21.7%, respectively. They said that there is no
specificity among acupuncture points. As we
mentioned above, the failure for them to find
relative specificity among acupuncture points could
well be due to low treatment frequency in this
study.
|
10.2. Between acupuncture points and non-points
It was reported that acupuncture on different acupuncture
points, or using different acupuncture technique, the
healing effects are similar. Some other studies showed that
acupuncture on traditional acupuncture points or on
non-points, the healing effects were similar.
Berman BM (2004)
allocated 336 patients suffering from osteoporosis of knee
joint into two acupuncture groups: acupuncture on points
that are normally used for the treatment of osteoporosis of
knee joint (acupuncture group, 173 cases), and that on
non-points (non-point group, 163 cases). The acupuncture was
twice a week for 8 weeks, then once a week for two weeks,
again once every two weeks for 4 weeks (total 23 sessions).
WOMAC functional score was improved in the acupuncture group
much more than that in the non-point group, but not WOMAC
pain scale.
Melchart D (2005)
randomly
allocated 195 tension headache patients into two acupuncture
treatment groups: traditional acupuncture group (132 cases),
and non-acupuncture point group (63 cases). The acupuncture
was twice a week for 4 weeks, then once a week for 4 weeks.
After 8 weeks, the headache score reduced in the acupuncture
group by 47.2%, while that in the non-acupuncture points was
also 44.3%. No significant difference between the two
groups.
Assefi NP (2005)
randomly allocated 99 patients with fibromyalgia into four
acupuncture treatment groups: traditional acupuncture group
(25 cases), on non-point acupuncture group (24 cases),
acupuncture needle not inserted group (25 cases) and
non-specific acupuncture group (e.g. the acupuncture points
normally not used for the treatment of fibromyalgia, 25
cases). The acupuncture was twice a week for 12 weeks. They
found that the pain deduction rate in the acupuncture group,
the non-specific group, non-points group and non-inserted
group, were
21.4%,20.3%,41.1% and 33.8%, respectively. No significant
difference between each groups
[23].
Witt C (2005)
randomly allocated 224 patients who suffered from
osteoarthritis of the knee into two acupuncture treatment
groups: acupuncture group (150 cases) and non-acupuncture
point group (74 cases). The acupuncture was twice a week for
4 weeks, then once a week for 4 weeks. After the treatment,
the pain reduced by 62.4% and 51.5% in the acupuncture group
and in the non-point group, respectively, without
significant difference.
Macklin EA (2006)
treated primary hypertension by acupuncture and said that
the healing effect is similar in the acupuncture group and
the non-point group. We noticed that the acupuncture was
performed in this study was twice a week. While for the
treatment of hypertension in China, it is mostly once a day,
even twice a day for 28 days.
Cabrini L (2006)
randomly allocated 32 patients undergoing branchofiberoscope
into two acupuncture groups, both were performed 20 min
before the surface anesthesia: acupuncture on traditional
points (acupuncture group, 16 cases), and that on non-points
(non-point group, 16 cases). In both groups, the needles
were kept until the end of the exam. The results showed
that, after acupuncture for 20 min, the anxiety level was
reduced by 42.7% in the acupuncture group, but did not
change in the non-point group.
The studies above are mostly done with
acupuncture once a week or
twice a week, rarely three times a week. The difference
between the acupuncture group and the non-point group are in
most time insignificant. When the acupuncture was performed
with higher frequency of treatment, the difference between
the two groups tended to be significant. Such data are
mostly from China.
万明雨
(2014)
randomly allocated 28 patients with primary migraine
(hyperactivity of liver-Yang type in TCM) into two
acupuncture treatment groups: acupuncture group (14 cases),
and other-points group (points that are normally not used
for the treatment of migraine, 14 cases). The acupuncture
was once a day for 10 days. The number of points in both
groups was the same (4 points). After the treatment, the
pain level was reduced in the acupuncture group and in the
other-point group was 50.0% and 26.2%, respectively.
章海凤
(2013)
randomly allocated 59 migraine patients into two acupuncture
treatment groups with the same numbers of acupuncture
points: acupuncture group (30 cases) and non-acupuncture
point group (29 cases). The acupuncture was once a day for 5
days. Have a two-day break between healing courses. It was
totally 4 courses. They found that the pain was reduced by
42% and 10.4%, in the acupuncture group and in the non-point
group, respectively.
张智龙
(2007)
[1080]
randomly allocated 255 constipation patients into two
electrical acupuncture treatment groups: acupuncture group
(126 cases) and non-point group (129 cases). The acupuncture
was once a day for 28 days. The result showed that the
electrical acupuncture treatment can dramatically improve
the symptom, speed up the content passing speed inside
intestine, reduce the usage of Constipation Relief
Suppositories Glycerol and evacuant. The total effectiveness
rate in the acupuncture group was 94.4% and that in the
non-point group, 61.3% .
樊莉
(2005)
randomly allocated 53 depression patients into two
acupuncture plus auricular acupressure treatment groups:
acupuncture group (28 cases) and non-point group (25 cases).
Acupuncture was twice per week for 3 months. After
treatment, the cure rate and the much-improve rate in the
acupuncture group was 28.6% and 28.6%, respectively, while
those in the non-point groups, 8.0% and 20.0%, respectively.
Chou CY (2005)
randomly allocated 40 patients with later stage of uraemia
with itch into two acupuncture treatment groups: acupuncture
group (20 cases) and non-point groups (20 cases).
Acupuncture was three times a week for one month. They
reported that the itch level was reduced by 54.7% and 2.6%,
in the acupuncture group and in the non-point group,
respectively.
The results of some studies that also compare the healing
effect of acupuncture group and the non-point group
was cited as not support the relative specificity between
acupuncture points. But actually they are not a proper study
to function as such. For example in the study by Vickers AJ
(2005),
they used non-inserted needle, not the inserted needles into
the skin.
Also in the study by
Scharf HP (2006),
the
used acupuncture points or non-points is together with
physiotherapy. It is hard to evaluate the actual amount of
healing effect in a mixed treatment program. Again, both
acupuncture and manual therapy of the physiotherapy are much
depending on personal skill. The overall healing effect
could be even more largely variable. Again, in the Western
style of physiotherapy, the practitioners usually ask client
to do physical exercise, while in Chinese acupuncture, we
ask patients stop physical activity whenever the pain is
very severe. Too much physical activity would make the pain
worse, rather than better. The way of the treatment and the
requirement to patients are quite different among these two
therapies.
10.3. Between different acupuncture techniques
There are many studies in China compared the healing effect
of acupuncture by its ordinary technique or by its various
modified techniques.
梅麟凤
(2008)
randomly allocated 56 patients who suffered from coma
due to severe cerebral trauma into two acupuncture treatment
groups: one is with comprehensive combined treatment
(including scalp acupuncture, auricular acupuncture and body
acupuncture, 36 cases) and another with body acupuncture
alone (20 cases). The acupuncture was once a day. 10-day was
one course, with 3-day break between courses. They found
that the effective rate in the two groups was 69.4% and 40%,
respectively.
崔新华
(2005)
randomly allocated 100 persistent vegetable states patients
into two acupuncture treatment groups: one was with ordinary
acupuncture (50 cases), and another was with special
acupuncture technique (50 cases). The acupuncture was twice
a day for 24 sessions. They found that the wake-up rate in
the two groups were 62% and 86%, of significantly different.
睢明河
(2012)
randomly and blindly allocated 293 patients of high blood
pressure into different treatment groups. This is one time
acupuncture. They found that, though the control group (in
this group the patients do not feel Deqi sensation) showed
some deduction of blood pressure, the blood pressure
deduction was much more in the Deqi acupuncture treatment
groups.
In the above studies in the comparison between a special
acupuncture technique and a conventional acupuncture
technique, the common characteristic of them is that they
are real and inserted treatment. This means that, the group
that was used as a control (the ordinary acupuncture group),
can also be regarded as a sham group (though it is not a
perfect sham, because it has its own healing effect too).
The similarity between the two groups is that both are
performed with the same treatment frequency and same level
of emotional influence to the patients. However, readers
might still question that the number of acupuncture points
used, the amount of stimulation to the points, all are
different between the two groups, so that the placebo effect
might be more in the group, in which more number of
acupuncture points were used, and stronger simulation was
given.
For this question, we can also show some other studies, in
which the kind of acupuncture points, the number of the
points, and treatment frequency between the groups, were
exactly the same. The differences between the groups are the
direction of needles after they are inserted into the point.
It sill showed that the acupuncture of special technique
worked better than a conventional acupuncture.
孙懿君
(2015)
randomly allocated 200 patients with cervicalspondylotic
radiculopathy into two acupuncture treatment groups: one was
with conventional treatment (100 cases) and another with a
special acupuncture technique (100 cases). The acupuncture
was once a day. 10-session was one course for total 2
courses. They found that the pain level reduced by 79% and
45.4%, respectively in the special group and in the
conventional group.
尚艳杰
(2011)
randomly allocated 64 patients with shoulder periarthritis
into two acupuncture treatment groups: one was with a
special acupuncture technique (32 cases), and another with
conventional technique (32 cases). The acupuncture points
used were the same, and the acupuncture was done once a day
for 6 days, with one day break before next course, for total
2 courses. They found that the cure rates were 53.1% and
31.2%, in the special acupuncture group and the conventional
group, respectively.
时晓燕
(2014)
randomly
allocated 150 stomach pain patients into three acupuncture
groups: special acupuncture technique I (special group
I, 50 cases), special acupuncture technique II (special
group II, 50 cases), and conventional acupuncture
(conventional group, 50 cases). They used the same
acupuncture points, but the different ways of manipulating
the needles. The acupuncture was once a day for one week.
They reported that the effective rate was 96%, 94%, and 60%,
in the special I, special II, and the conventional group,
respectively.
李伟
(2015)
randomly allocated 160 patients who suffered from prolapse of lumbar
intervertebral disc into two acupuncture treatment groups:
special acupuncture technique (Wen-tong technique, 80 cases)
and conventional acupuncture (80 cases). The acupuncture
points used were the same. The acupuncture was once a day,
15-day as a course. They reported the excellent healing rate
was 97.8% and 78.8% in the special acupuncture group and the
conventional group, respectively.
陈美仁
(2007)
randomly
allocated 165 sciatica patients into two acupuncture
treatment groups: one was with a special acupuncture
technique (special group, 82 cases), and another with
conventional electrical acupuncture technique (83 cases).
Both groups used the same acupuncture points. The
acupuncture was performed once every other day. Ten-session
was one healing course. They reported that the
cure-much-improved rates in the special group and the
conventional group were 88.7% and 57.5%, respectively.
10.4. Different influence of acupuncture and
pseudo-acupuncture
A lot of studies have indicated that there happened many
neurohumor changes in the body after acupuncture, but no
such changes with a sham acupuncture (or a
pseudo-acupuncture). For example, acupuncture can induce
secretion of some nerve-chemical substances, such as
Beta-Internal polyphenol,
enkephalins, and serotonin.
Animal studies showed that acupuncture can change the
transportation of nerve transmitter, such as opioid and
monoamines in the brainstem, cerebral ganglia, hypothalamus
and hypophysis.
Therefore it is
deduced that acupuncture can work through changing the
autonomic nervous system.
For example, electrical acupuncture can reduce the
sympathetic nervous activity.
Because those effects and changes could not be observed in
sham group, the effects of acupuncture treatment were
induced to be due to the stimulation of acupuncture points
or meridians.
If acupuncture is merely a placebo effect, how could be the
difference between different acupuncture point(s), between
acupuncture point and non-point, between different
acupuncture techniques, and between different manipulating
technique on the needle in the same acupuncture point?Also
how can acupuncture stimulate various hormone secretion but
the sham acupuncture not? In fact, the above comparison
studies are reproducible. It should be pointed out again
that these results were obtained with frequent acupuncture
treatment schedules, e.g. the acupuncture was performed
mostly once a day, or at least once every other day. If it
is performed as once or twice a week, they may be hard to be
reproduced.
Brief summary:
Another way to test if an acupuncture treatment is a placebo
effect is to compare the healing effect between different
acupuncture points, between acupuncture points and
non-points, between different acupuncture techniques, under
the same experimental conditions. Again, such comparison
must be compared with higher treatment frequency. In low
treatment frequency, such comparison might or might be
significantly different. In higher treatment frequency, it
tended to be statistically significant. This is additional
evidence that acupuncture is not a placebo effect.
Chapter 11. More examples that acupuncture is not a placebo
effect
We have already discussed why
Colquhoun D
could make a summary that acupuncture is only a placebo
effect, because the acupuncture in the studies that he cited
are not the kind of acupuncture in clinic in China. What he
means the acupuncture is not what we mean the acupuncture.
We can cite more evidence that acupuncture is not a placebo
effect, such as acupuncture used in children and in animal.
11.1. Acupuncture in children
Acupuncture can not only be used to treat diseases in adult,
but also those in nursling
and children.
It can be used for the treatment of various diseases
including various pain,
migraine,
infant catatonia,
bedwetting,
constipation,
allergic rhinitis,
saliva incontinence,
spastic paralysis,
laryngismus,
postoperative vomit,
nausea/vomit after chemotherapy
and so on.
Ecevit A (2011)
reported that, by only acupuncture on Yintang point, it can
reduce the pain level in premature with the pain in heels
due to blood sample taking for analysis. The crying time can
reduce from average 138.1 seconds down to 72.8 seconds. At
the same time, the heart rate reduced from 152.2 times per
min down to 138.3 times per min. The pain index reduced from
6.1 down to 4.2, suggesting that the tolerance of the
premature to pain increased.
Liodden I (2011)
did acupuncture to 77 children undergoing tonsillectomy and
adenoidectomy. The acupuncture started after induction of
general anesthesia on Neiguan points. The needles were taken
out before wake-up of the children and a plastic needle was
put on the same points for 24 hours (covered) . There was
another group as a sham group. It was found that the
incidence of postoperative nausea/vomit in the acupuncture
group was 46.8% but that in the sham group, 66.2%. It is
interesting that the incidence in the children aging 1-3
years of old (26.7%) is less (59.6%) than that in older
children (4-11 years of old). Generally speaking, we should
expect that the older children of 4-11 years of old should
be more affected by the placebo effect of treatment, but the
results here showed opposite. The possible explanation is
that the acupuncture stimulation in the younger children
group is relatively more than that in the older children.
A survey in North America for 43
children hospitals showed that, about one third of the
hospitals supply acupuncture treatment
.
Most of other studies said that the number of children who
are suggested to use acupuncture treatment is also large.
Generally speaking, the parents of the children also
accepted this therapy and satisfied the healing effect.
This is quite different from most of people thought, since
generally speaking, children may fear the needles,
and the parents may not want to increase pain and fear to
the children
The age of the children who accepted acupuncture treatment
can be as little as one month.
For so youth children, how can we expect that the baby can
accept a placebo effect?
Weimer K
(2013)
had a review, from which we know several other reviews about
placebo effect in children and adolescence. We learned that
the placebo responder rate is generally higher than that in
adult, that the mechanisms behind the placebo effect in
children might be different from that in adult, and that the
clinic study design in children might need to be different
from that in adult too. However, it seems that it is very
rare that the studies included paid attention to compare
children younger than one year old with those age more than
, for example, 6 years or 12 years of old. We suspect that,
the placebo responder rate and placebo effect in these
groups might be different.
Someone may believe that the placebo effect can also happen
in children younger than 2 years of old.
However, this is not accepted by others, the later suggested
that the placebo effect in such younger children might be
due to the parent placebo effect, as proxy-placebo effect,
which cause the bias report in the younger children.
11.2. Acupuncture on animal
If we are still not convinced by data of acupuncture on
children, and still suspect that the acupuncture effect is a
placebo effect, let us see the animal studies on
acupuncture. Acupuncture not only works in human being, but
also on animals. A lot of clinic studies supported this.
Gakiya HH (2011)
randomly
allocated 30 dogs undergoing mastectomy into three groups.
One is electrical acupuncture group, one is sham group, and
another is no-acupuncture control groups. Each group is 10
dogs. After the treatment, the number of dogs that need pain
killer in the electrical acupuncture group, the sham group,
and the non-treatment group was 2, 6, and 6, respectively.
They summarized that acupuncture could reduce the
postoperative consumption of morphine and
promote satisfactory analgesia
in dogs undergoing mastectomy.
Cho SJ
and Kim O (2008)
did acupuncture for a dog suffered from cervical sympathetic
paralysis syndrome, once a day for two days. After two days,
all the symptoms disappeared. (This data suggested that
acupuncture everyday worked better).
Ceccherelli F (1996)
randomly allocated rats into three groups: acupuncture group
(14 cases), morphine group (10 cases), and non-treatment
control (20 cases). They found that acupuncture can
significantly reduce the experimental swelling in the feet
of the rats. Data from
Zhang RX (2005)
reported
similar findings.
Carneiro ER (2010)
randomly allocated rats into acupuncture group, non-point acupuncture
group, activity-limited group, and no-treatment group.
All rats were sensitized with
heat-solidified hen egg white implant. Using clinical
acupuncture points, EA treatment began 2 days after antigen
priming and was repeated on alternate days for 2 weeks. They
found that electrical acupuncture efficiently diminishes the
bronchial immune-mediated inflammation induced in rats and
that this effect is dependent on the choice of specific
acupoints.
Luna SP
(2015)
had a study on dogs undergoing
ovariohysterectomy. They found
that acupuncture
or pharmacopuncture were equally effective as morphine or
carprofen to control postoperative pain in bitches
undergoing ovariohysterectomy.
Cassu RN
(2008) compared
the analgesic effect of uni- and bi-lateral
electroacupuncture in response to thermal and
mechanical nociceptive stimuli and investigated the
cardiorespiratory, endocrine, and behavioral changes in dogs
submitted to
electroacupuncture. They
found that bilateral
electroacupuncture
produced a shorter latency period, a
greater intensity, and longer duration of analgesia than
unilateral stimulation, without stimulating a stress
response. The effect of electrical acupuncture for pain
reduction was confirmed by their later studies again.
Although
Gakiya HH
did not find difference between the acupuncture group and
the non-point group for the pain level reduction, but they
did find that the pain killer used in the acupuncture was
less than non-acupuncture group.
Groppetti D (2011)
found that plasma
β-endorphin levels in dogs receiving electroacupuncture
increased significantly against baseline values after 1 and
3 h after surgery. Moreover, the end-tidal isoflurane
concentration needed for second ovary traction was
significantly lower in acupuncture-treated dogs than control
animals. All animals having electroacupuncture experienced
prolonged analgesia, over 24 h at least, while four out of
six dogs treated with butorphanol needed post-surgical
ketorolac and tramadol supplementation to their pain relief.
Koh RB
(2014)
studied the effects
of maropitant, acepromazine, and electroacupuncture on
vomiting associated with administration of morphine in dogs.
They found that
maropitant
treatment was associated with a lower incidence of vomiting
and retching, compared with control treatments, and
acepromazine and electroacupuncture appeared to prevent an
increase in severity of nausea following morphine
administration in dogs.
Jaeger GT (2006)
reported their study: seventy-eight dogs with pain due to
hip dysplasia were studied in a controlled, double-blind
clinical trial to evaluate gold bead implantation as a
pain-relieving treatment. The dogs were randomly assigned to
two groups, 36 in the gold implantation group and 42 in the
placebo group. Both groups were treated equally regarding
anesthesia, hair clipping, and penetration of the skin with
the same type of needle. The gold implantation group had
small pieces of 24 carat gold inserted through needles at
five different acupuncture
points and the placebo group had the
skin penetrated at five non-acupuncture points so as to
avoid any possible effect of stimulating the acupuncture
points. A certified veterinary acupuncturist marked the
points, and two surgeons performed the implantations
according to a randomization code made in advance. After 14
days, three months and six months, the owners assessed the
overall effect of the treatments by answering a
questionnaire, and the same veterinarian examined each dog
and evaluated its degree of lameness by examining videotaped
footage of it walking and trotting. The treatment was
blinded for both the owners and the veterinarian. There were
significantly greater improvements in mobility and greater
reductions in the signs of pain in the dogs treated with
gold implantation than in the placebo group. The
veterinarian’s and the owners’ assessments corresponded
well.
Laim A
(2009)
studied the effects of adjunct electroacupuncture on
severity of postoperative pain in dogs undergoing
hemilaminectomy because of acute thoracolumbar
intervertebral disk disease.
Dogs were alternately assigned to treatment (conventional
analgesics and adjunct EAP) and control (conventional
analgesics alone) groups. Analgesic treatment was adjusted
as necessary by the attending clinician, who was not aware
of group assignment. They found that
total
dose of fentanyl administered during the first 12 hours
after surgery was significantly lower in the treatment group
than in the control group, though dosages of analgesics
administered from 12 through 72 hours after surgery did not
differ between groups. Pain score was significantly lower in
the treatment group than in the control group 36 hours after
surgery, though did not differ significantly between groups
at any other time.
Some people explained the healing effect of acupuncture in
animal as conditioning. Due to a repeated conditioning,
animals could also have psychological and physiological
responses, so as to have improvement in their symptoms. For
example, to bring a dog to a veterinary station, the dog may
shack in body. This might be because the dog had been
brought to the station before and suffered from pain
stimulation, such as injection. If bring the dog to quiet
and peace environment, the dog could show less level of the
symptoms. This might be easy to understand.
For this, Ramey D
explained that
conditioning theory proposes that
bodily changes result following exposure to a stimulus that
previously produced that change. This is perhaps the most
intuitively acceptable explanation for any placebo effects
in animals. Indeed, animal studies support such a model for
placebo effects, starting with the first descriptions on
salivating dogs by Pavlov. Both human and animal studies
support the idea that conditioning forms some basis for
placebo responses. Since conditioning requires learning, it
would be expected that repeated visits to a practitioner (of
any particular persuasion) might increase the strength of
the association between a learned stimuli and response in
animals, good or bad. There are numerous examples of dogs
shaking in fear when being taken into a veterinary clinic;
on the other hand, a dog that enjoyed being handled in a
soothing environment might appear to receive some relief
from a chronic condition; as it learned to associate its
visits with the comforting handling, conditioning effects
could occur. This could certainly serve as reasonable
explanations for purported placebo effects in animals.
Nevertheless, the hypothesis that a healing or therapeutic
effect can be dependably provoked as a result of
conditioning cannot be supported at this time by any
evidence.
Expectancy theory proposes that bodily changes may occur to
the extent that the person receiving the therapy expects
them to. There is considerable overlap between expectancy
and conditioning, because learning is one of the major ways
that expectancies are formed. To the extent that therapies
are expected to provide relief from disease, or at least
provide the client and/or veterinarian with a feeling of
control over the disease process, they may alleviate adverse
mental states (in the humans). Certainly, in humans,
therapies that help restore patient control may evoke
therapeutic effects, at least short term, but studies that
investigate the expectancy model in animals have so far not
been performed. Still, if animals were able to form an
association between treatment-related signals (the attention
and handling received, the way that the owner behaves
towards the animal when it is receiving treatment) and the
relief of its distress, expectancies of treatment effects
might develop (on the part of both animal and owner).
There is a good body of research that demonstrates that
human contact has measurable effects on animals. For
example, petting by humans reduces heart rates in dogs and
horses and causes major vascular changes in dogs. Gentle
handling increases productivity in dairy heifers and
increases reproductive efficiency in sows. Thus, it is
plausible that human-animal contact might play an important
role in the observed responses to therapeutic interventions.
To take an “alternative” example, it has been shown that a
single acupuncture treatment is as effective as petting a
horse, when it comes to relief of signs of chronic airway
disease; that is, there’s no demonstrable effect of
acupuncture beyond simple handling. (9) On the other hand,
handling may also be stressful to animals, so responses to
handling may not necessarily be beneficial. Still, there’s
no question that human contact can invoke responses from
animals and animals may behave quite differently when they
are not being observed; those shouldn’t be confused with
placebo-effects, however.
It was reported that, after taking sedative, a dog was left
in a room but its owner left the room, then let a stranger
comes in the room, the dog showed quiet, rather than anxiety
or stressful as if it was not given a sedative before. On
the third time, the dog was given a vitamin, not a sedative;
again the coming in of a stranger in the room does not
create the same level of anxiety and stress reaction of the
dog. This experiment suggested that, once a therapy worked,
the following similar therapy or a sham therapy could
produce the same healing effect. Here, it should be noticed
that, precondition for such "replacing phenomenon" to happen
is that the previous therapy worked. While in the
experiments above, animal had acupuncture only once before
surgery. No previous healing effect for the dog to remember
in its brain.
It is the same in human being.
Goebel M (2008)
has a study. Patients
with allergic rhinitis underwent a conditioning protocol,
receiving desloratadine, an H1 receptor
antagonist, paired with a novel drink, for five consecutive
days. After the washout period, patients who were reexposed
to the novel drink plus placebo showed improved symptom
scores, decreased wheal size on the skin prick test, and
diminished basophil activation.
Numerous other pharmacological conditioning trials have
shown that these placebo responses mimic active drug effects
and that prior exposure to an effective treatment is an
important part of the conditioned placebo response.
08D0C9EA79F9BACE118C8200AA004BA90B02000000080000000E0000005F005200650066003400360037003100350034003600320031000000
However, no matter for the expectancy, conditioning, or such
replace effect, the animal needs a pre-experience to the
stimulation. For acupuncture treatment, the question is, the
acupuncture is only one time treatment, before the surgery,
and it worked to reduce the incidence of postoperative
nausea/vomit. The animal did not receive repeated
acupuncture. The expectancy, the conditioning, or the
replacement effect should not be established.
Another explanation is that the animal might get more care
after sick, they would become quiet and calm, and so the
symptom would be reduced. They explain this possibility as
broad concept of a placebo effect. However, this theory has
no any experiment to support, neither be able to answer how
much extent a care could calm down a symptom. In addition,
such care to calm down a symptom should not be confused with
what is discussed here the placebo effect.
Based on the current data, it is most possibly that, the
disease-treatment reaction in an animal is similar to that
in an infant or children. They are not easily affected by a
placebo effect (hint effect). They may be more affected by a
calm effect. That means that the reduction of a symptom in
an animal or in a child might become less after they get
care and conciliation from the owner or parents. They may
have reduced heart rate and reduced blood pressure. However,
the pain level may not really be reduced by such
conciliation. Such calm of animal or child might be regarded
as an evidence of a reduction of pain. But we, as adult,
know that, under conciliation, the emotion may become calm,
but the pain level may not really reduce.
Therefore, the results of acupuncture studies on animal or
on children support less as a placebo effect but some kind
of conciliation effect. If, under the conciliation, the
animal still is not willing to move, or a child is still
crying, it should be regarded as the pain level (symptoms)
is not improved yet. If, after acupuncture, the animal
starts more motion, or a child stop to cry, it should be
regarded that the symptom has been improved. Animal or
children belong to not-cheating group. We do not really need
to insist that the improvement of symptom after acupuncture
is an exaggeration of the improvement by owner or parents.
Brief summary:
Small children or animal is less
apt to a placebo effect. Especially for them, that only
one or two times of acupuncture treatment could reduce
their symptoms suggests that the healing effect of
acupuncture cannot be simply explained by a placebo
effect or a conditioning effect. The only explanation is
that acupuncture indeed has its own specific healing
effect.
Chapter 12. Why people made the comment that acupuncture is
a placebo effect
Now, we can see that there are several reasons that made
some of acupuncture researchers in the Western countries
believe that acupuncture is a placebo effect. Let us make a
summery for these possible reasons.
12.1. In the acupuncture studies in the Western world, the
difference in the healing effect between the acupuncture and
the sham group is not large
In the study reports from Western countries, the healing
effects of acupuncture group are in a low level. Therefore,
once the effect in the sham group is higher, it would be
easy to lose statistically significant between the two
groups.
Then the question is why the healing effect in the
acupuncture group is low in the studies reported in the
Western countries, compared with that reported in China?
According to the data we collected here, we believe that the
reasons might be the followings:
(1). Too low treatment frequency. Most of the studies
applied acupuncture once or twice a week in the Western
countries, while it is once a day or once every other day
(5-6 sessions per week) in China. The total course dose of
acupuncture in the Western countries is 3-4, while that in
China is more than 8. Too low stimulation of acupuncture
could not yield sufficient healing effect. It is needed for
the acupuncturists in the Western countries to visit
acupuncture researchers in China, to see how the
acupuncturist in China did acupuncture study and clinic work
there. They need to perform acupuncture the same ways as
acupuncturists in China, rather than a Western modified
acupuncture.
According to the current data, with higher treatment
frequency, the healing effect of acupuncture group tends to
be higher and that of a sham group, lower, so that it is
easy to yield a positive report. While with low treatment
frequency, the healing effect of acupuncture group usually
was not high (so many data showed this), while that in the
sham group tends to be higher, so it is easy to result in a
negative report. It was found that a negative report is easy
to happen in a study where the healing effect of sham group
is high. Therefore, we recommend that acupuncture should be
performed at a high treatment frequency, for most of
diseases. For some special diseases, even acupuncture once a
day is not sufficient. We have to use special acupuncture
technique, pay attention to proper involving time, etc. to
get higher healing effect. The examples for such diseases
are cancer, migraine, post-stroke coma, persistent
vegetative state, etc.
Why in the most of the studies in the Western countries, the
acupuncture was performed once or twice a week, instead of
five or six times a week? Most of the researchers mentioned
that the way of the acupuncture are referred from a
published article, or had consulted with an expert in
acupuncture. Very rarely they mentioned that they referred
from articles published from China. Language barrier might
be the most reason for this?
(2). Single or double blind design of the study. Such design
blocked the communication between the acupuncturist and the
patient. This makes it impossible for the acupuncturist to
know the feeling of the patients to the needle manipulation,
so it is hard for the acupuncturist to induce along-meridian
feeling to reach the highest healing effect. The
acupuncturist would also feel hard to get response from the
patients so as to be able a change the treatment schedule or
the way of the acupuncture to match the individual need for
the treatment.
For this reason, we say that this is a researcher-modified
acupuncture. It is not a "real" and "clinical" acupuncture.
It is an "imaged" acupuncture in the acupuncture researchers
in the Western countries.
(3). The personal skill of acupuncturist is not
guaranteed. For a therapy that depends mostly the
personal skill, if the person is not good enough
skillful, the result of a study can be expected not
good.
12.2.
Comparing between different treatment frequency, between
different acupuncture points, between acupuncture points and
non-points, between different technique, no significant
difference
Generally speaking, there are not many studies to compare
these different groups. But once there is such comparison
study, its influence is very big to the research society.
Among them, one is the study by Yuan J (2009),
who compared two treatment frequencies: twice a week for
five weeks and once a day for five day per week for two
weeks. The author did not find difference between the two
groups.
However,
they used moxibution and cupping together with the
acupuncture. It was a comprehensive treatment, not
acupuncture-alone comparison. It can only mean that, with
the combination of other therapies as in real clinic
situation with moxibustion or cupping, the acupuncture
treatment can be done twice per week. Also in this study,
the healing effect in the 5-session group was better than
the 2-session group in the treatment of severe cases.
Moreover, the healing effect in the 2-session group stayed
no more improvement in the following weeks, but the
treatment in the 5-session group may have further more
improvement if the treatment was continued in more weeks.
This means possible that after five weeks, the healing
effect in the 5-session group might be better than the
2-session group.
There is only
limited number of such comparison studies in the Western
countries, and they were mostly performed at low treatment
frequency, so that it is easy to get negative reports
showing that there was not difference between the
comparisons. This easily brings people to create an wrong
impression that acupuncture does not depend on proper choice
of acupuncture points, not on the Deqi feeling, not on
treatment frequency either.
There
are lots of comparison studies in China however (see above)
and they are mostly performed at high treatment frequency.
Their results clearly showed difference between the compared
groups. This is one of the major reasons for acupuncturists
in China do not believe that there is no relative
specificity between acupuncture points/meridians, and that
the non-point could work evenly to, or even better than, a
typical acupuncture point.
12.3. Simply contribute the most part of the healing effect
in the acupuncture group into a placebo effect, only a small
part into the acupuncture specific effect
Generally, it is believed that the total healing effect
of an acupuncture group is the sum of the acupuncture
specific effect and the placebo effect(deduced
from sham group). Therefore, if
we know the amount of healing effect from a sham group, we
can get the amount of the specific acupuncture effect by
deducting the sham effect from the total effect in the
acupuncture group. This consumption omits a common
phenomenon: when two or more therapies are used the same
time, the total effect is usually not the sum of the healing
effect of each therapy when they are used alone, no matter
the placebo effect has been deducted from the total effect
or from each of the therapy or not. Therefore, in the
acupuncture group, we cannot tell exactly how much is sham
and how much is the contribution of the acupuncture specific
effect, even if we know the amount of the sham group.
Current way of estimation of acupuncture specific effect in
the acupuncture group underestimated it.
12.4. Improperly choose acupuncture points, contribute its
low effect to that of acupuncture
Some researchers heard that acupuncture point Neiguan can be
used to treat nausea or vomit; they then use this point to
treat nausea/vomit of any reasons, such as postoperative
nausea, post-chemotherapy/radiation therapy nausea, and so
on. They also observed the healing effect of only one such
acupuncture point, rather than used more other complementary
points according to different reasons for the symptom. If
the acupuncture they tried this way does not work, they will
comment that acupuncture does not work.
Chang CH
(2005)
used electrical acupuncture on the Zusanli points of healthy
volunteers, to see if the acupuncture could adjust the heart
rate after the person was given atropine. The result was
that there is no effect. In TCM theory, the acupuncture
meridian that may affect heart function mostly is the Xin
Jueyin meridian, especially the Neiguan points. The Zusanli
point used in this study belongs to Stomach meridian. We
normally do not use this point to affect the heart rate or
heart function. Therefore, the result of such study should
not be regarded as evidence that acupuncture does not work.
Cho CY (2005)
treated
refractory skin itch due to late stage of uraemia with
acupuncture. Although it was showed that the healing effect
of the acupuncture group was higher than the sham group,
this study might be hard to be reproduced by other
researchers. This is because the patients were in late stage
of disease. The basic reason for the skin itch remained not
change during and after acupuncture treatment. Also, the
acupuncture was three times per week for one month. It is
not a high-reproductive study design for acupuncture
treatment. The positive result in this study is very much by
a chance.
12.5. Study on a disease that is not in the working scope of
acupuncture treatment
Acupuncture is only one of the therapies, not the main
therapy in Chinese medicine used in China. It can be used
for the treatment for some kinds of diseases, but as any
types of therapy, not for all kinds of diseases. This is the
same as for Western medicine. For example, Western medicine
cannot solve the AIDS. We cannot therefore deduce that the
Western medicine does not work. For the acupuncturists in
the Western countries, it is not proper to study the
diseases that are not in the list of recommended list of
diseases for acupuncture treatment (by acupuncturists in
China). Otherwise, the failure of the trial can be
summarized as that acupuncture does not work for the disease
tested (in the authors’ hands), but not that acupuncture
does not work.
Some diseases might not be proper to
use acupuncture for the treatment, at least for the
movement, or for most of the acupuncturists, such as
fibromyalgia.
Patients
with fibromyalgia are very sensitive to skin touch[25].
They cannot tolerate even slight touch on this tender skin,
not to speak of the needle insertion and the Deqi feeling.
For this reason, that some studies showed negative results
should not be regarded as acupuncture not work for any other
disease condition .
12.6. Confuse the healing effect of cupping, moxi,
electrical acupuncture, auricular acupuncture, TENS,
massage, all as acupuncture
Indeed, all of these therapies belong to traditional Chinese
medicine and used in acupuncture clinic broadly. But each
therapy has its own proper way to use and with favorite
disease scope. To include their healing effect into that of
acupuncture is not a proper way. Acupuncture may work better
than them, or not, depending on many things.
In many review articles on acupuncture these various
therapies are involved into the review as acupuncture. For
example they are included in the review by
Colquhoun D,
Furlan
AD (2010)
and
by Linde K (2009).
Therefore,
in our article here, we tried to separate the healing effect
of acupuncture from that by other therapies. Acupuncture can
work by itself, not always need to be combined with other
therapies to exercise healing effect.
Liu WH
(2015)
had a review about acupuncture. They collected randomly
designed articles from year 2011 from
Science Citation Index Expanded
(SCIE), excluded those published from China, or the first
author is from China. By this way, they got 33 articles from
totally 867 articles. Among these, 17 articles are negative
and 23 articles are positive. From the 33 articles, we could
remove the studies using electrical acupuncture, auricular
press, auricular acupuncture, or finger press,
acupuncture injection or cupping,
acupuncture being not the main therapy,
only paying attention to the treatment cost changes,
observing the residence days and cost of acute disease (Painovich
J),only
observing long term healing effect,
and
wrong summary for the study results (such as to comment a
negative result as a positive result).
Then, the negative articles become 7, and positive articles,
14.
Azad
A (2013)
listed 25 so called negative articles about acupuncture.
Among them, there are 8 articles that used intradermal
needling, acupuncture point press, auricular press, or
magnetic therapy. The diseases treated by acupuncture are
four categories: the fatigue and hot flash due to cancer or
due to chemotherapy, or postoperative pain (8 articles);
nausea/vomit after chemotherapy (5 articles), xerostomia
after chemotherapy or radiation therapy (3 articles), and
leucocytopenia after chemotherapy (1 article).
In the first category, the acupuncture was mostly done once
or twice a week. Only one study was three times a week.
Among this, clearly positive articles are 5,
,
and negative results are 2 articles (both are acupuncture
once or twice a week).
While
in one article, some parameters were positive and others
were negative.[1149]
In the 8 articles, the healing effect in the sham group was
average 12%±16%, but that
in the acupuncture group (including 2 electrical acupuncture
groups) was 35%±19%, higher
than the sham group.
In the Azad A (2013)
review, in the articles about nausea/vomit after
chemotherapy or radiation therapy, 2 articles are positive,
3 are negative
in
which 2 articles are the same author,
the basic data and summary are exactly the same). In the
articles about xerostomia after
chemotherapy or radiation therapy, 2 articles are positive,
another article is partly positive and partly negative.
The one article
about
leucocytopenia after chemotherapy is positive: acupuncture
can increase blood number of white blood cells.
Therefore, in
the 25 articles cited by Azad A (2013)
review, only 4 articles can be used as negative to
acupuncture. For the diseases studied by these 4 articles
(the side effects of chemotherapy and/or radiation therapy),
there are also a lot of positive studies against their
negative results.
Apparently, in the current review articles, there are many
non-acupuncture studies. This is a common phenomenon of the
review articles in the Western countries. They regard such
largely variable therapies all as acupuncture.
12.7. Superstitious belief
on large scale experiments
Theoretically, in a clinic study, the
larger the sample size, the more believable the results are.
This
can be verified in Western drug studies, but may not be so
in studies on acupuncture.
The reason is that, in the drug studies, the kind, the
quality and the quantity of the drug can be and is
standardized. For example in the study of Aspirin in the
prevention of cardiovascular diseases, the Aspirin produced
in US and in Germany is believed the same quality. The
Aspirin used US and China is not doubted to have any big
difference. The difference is the people who receive it, for
example the age, sex, history of diseases, history of
smoking, habit of diet, etc.
While in acupuncture studies, beside the variations from the
receiver, even if the choose of acupuncture points, the
number of the points and the treatment frequency, are all
the same, the personal skill among the acupuncturists could
still be largely variable. Such operator’s variation is not
easy to control. Therefore in large scale acupuncture, when
the study involve large number of acupuncturists and large
number of clinics or hospitals, the results of the study
would tend to narrow
the difference in the healing effects between the
acupuncture group and the sham group, so as to produce a
negative summary. While in the acupuncture study, as in
other medical studies, the data from a large scale study is
highly praised.
12.8.
Co-exit of opposite ways in acupuncture treatment
In the acupuncture treatment, there are some quite different
or opposite ways to handle the needle or to choose
acupuncture points. It seems that both works and this
phenomenon is very difficult to understand. Even for us, we
cannot explain all of the opposite ways but both works. For
example, we focus on the deep insertion of the needles, but
there are also some other styles of acupuncture in which the
needle is asked to insert in shallow, such as in Wrist-ankle
acupuncture, floating acupuncture, or some Japanese shallow
needle acupuncture; we use body acupuncture, in which we may
choose acupuncture points in any part of the body, but we
may also only use local acupuncture technique, in which the
acupuncture points are chosen from a very small part of the
body, such as from one ear, one eye, the nose, the tongue,
one hand, or one feet. The acupuncture point chosen can be
only one point, such as the Neiguan point than is used in
the treatment of nausea/vomit, or we may need to choose many
acupuncture points for the treatment. We may need only one
time acupuncture treatment but we may need many times of
treatment. We said that the acupuncture needle should be
inserted into a so called acupuncture point, but it may also
work if the needle is inserted into a non-point. The
acupuncture points might be chosen from the sick side of the
body, or from non-sick side of the body; or from upper part
of the body, or from lower part of the body; or from local
points, or from distance points. It is said it should be
considered to choose the first acupuncture point according
to the time of the day (Zi Wu Liu Zhu), but it apparently
not needs to be so.
All of these discrepancies certainly bring people to
question if acupuncture is a placebo effect, because this is
the simplest and easiest way to explain all of these
discrepancies.
12.9. Not care or omit large amount of positive results
Almost in all diseases studied in the Western countries on
acupuncture, there are some amounts of negative studies, but
also a large amount of positive studies too. If we include
those articles published in China, the number of positive
studies is much larger.
Acupuncture is only one of the therapies, not at all the
main therapy, in Chinese medicine used in China. It can be
used for the treatment for some kinds of diseases, but as
any kind of therapy, not for all of the diseases. This is
the same as for Western medicine: Western medicine cannot
solve the AIDS; we cannot therefore deduce that the Western
medicine does not work. For the acupuncturists in the
Western countries, before it has been established that
acupuncture worked for treatment of diseases, as reported
from China, it is not proper to study the diseases not in
the proper recommended disease list by acupuncturists in
China, and to contribute the negative result to acupuncture.
When in a study, negative and positive data showed up again
and again, it suggests that there is some factor(s) that we
have not realized and that really affect the reproducibility
of the study. If one study cannot reproduce the data of
another one, especially in the study of acupuncture, it
might be due to the difference in the study design, the
steps of the study, or the personal skills. The reviewers,
if he or she is really qualified scientific researcher, must
be very careful and patient to make a conclusion, not just
push the 3000 articles out of the desk to leave for coffee.
After
we collect more
data, especially those from China, we can easily find the
difference in the way of acupuncture between Western
countries and China. In China, high frequency of acupuncture
treatment may be associated with high healing effect, while
a relatively low treatment frequency is associated with
unstable results (positive or negative). It is needed for
acupuncturists in the Western countries to test the
acupuncture effect with higher treatment frequency.
Brief
summary:
There are many reasons that make the acupuncturists in the
Western countries believe that acupuncture is a placebo
effect. Most importantly is the low healing effect in
acupuncture group, which is due mostly to the low treatment
frequency by acupuncturists in the Western countries.
Chapter 13. Argue about acupuncture on the internet
During collection of data for this article, we found that
many people have already affirmatively believed that
acupuncture (and many other kinds of alternative medicine)
is a placebo effect.
There are
cut-throat discussions about whether the acupuncture is a
placebo or not; if the clinic doctor should use positive
placebo to patients or not; and if a medical study should
involve a sham group or not, and so on. The argument is big
as a sea wave on the internet.
The representative who believes that acupuncture is a
placebo is Colquhoun D.
He believes that the healing effect of acupuncture group and
the sham group is similar. Even if some study showed that
acupuncture is significantly higher than sham group, it is
only about 10% higher, which is not big meaning to clinic
work. To enhance his argument, he gave an example that "Although
it is commonly claimed that acupuncture has been around for
thousands of years, it has not always been popular, even in
China. For almost 1000 years, it was in decline, and in
1822, Emperor Dao Guang issued an imperial edict stating
that acupuncture and moxibustion should be banned forever
from the Imperial Medical Academy. "
He also commented that "
Acupuncture continued as a minor fringe activity in the
1950s. After the Chinese Civil War, the Chinese Communist
Party ridiculed Traditional Chinese Medicine, including
acupuncture, as superstitious. Chairman Mao Zedong later
revived Traditional Chinese Medicine as part of the Great
Proletarian Cultural Revolution of 1966.2 The
revival was a convenient response to the dearth of medically
trained people in postwar China and a useful way to increase
Chinese nationalism. It is said that Chairman Mao himself
preferred Western medicine. His personal physician quotes
him as saying “Even though I believe we should promote
Chinese medicine, I personally do not believe in it. I do
not take Chinese medicine.”"
He believed that
"The political, or perhaps commercial, bias seems to still
exist. It has been reported (by authors who are sympathetic
to alternative medicine) that “all trials [of acupuncture]
originating in China, Japan, Hong Kong, and Taiwan were
positive.”
People in other websites who argue against acupuncture as a
placebo effect but cannot answer why acupuncture study in
China, Japan and other Asian countries showing high healing
effect in acupuncture group, and why even in the Western
countries, the number of positive study is much more than
that of negative study.
Apparently Colquhoun D
knew that acupuncture studies from Asian countries are more
as positive to acupuncture, but he did not spend time to
check why more positive results are from acupuncturists
there. He did not pay attention that acupuncture in these
countries is with higher treatment frequency than that in
the Western countries. This might be understandable, that he
may not know Chinese. Even most of the acupuncturists in the
Western countries do not know Chinese either. They do
acupuncture as their imaged way. The question is:
acupuncture is created from China; acupuncturists in China
claimed that it works but the acupuncturists in the Western
countries cannot reproduce it, then, why they do not check
how acupuncture experiment was performed by acupuncturists
in China?
About the attitude of a historical figure to acupuncture
should not be used as supporting evidence. In Chinese
history, there were so many emperor, who supported or at
least not oppose against acupuncture, how comes only the
Emperor Dao Guang is so clear to know that acupuncture does
not work? Emperor Dao Guang was not a doctor or not an
acupuncturist. If the attitude of a nonprofessional man can
be used as supporting evidence, the attitude of a
professional man should be more convinced. Doctor Robert S.
Mendelsohn published a book named《Confessions
of a Medical Heretic》.
In the book, the author argued against many Western medicine
therapies. If we should trust layman Emperor Dao Guang,
shouldn't we more trust doctor Robert?
To take Chairman Mao's attitude as supporting evidence is
neither proper. He is for sure one of the greatest in
Chinese history, but he is also a human being. He also
committed big mistake, as he started the Great Cultural
Revolution. In the early time of New China, the Western
medicine was dominant in China too. Its healing effect is
indeed very high; we have no reason not to use it. However,
the country was very short of medical doctors, as well as
the Western medicine. To solve this, Chinese government
tried some ways, including training Western medicine doctor
to learn Chinese medicine as well. It means that the Chinese
government admitted the usefulness of the Traditional
Chinese Medicine. That previous policy is even correct
nowadays. For example, currently many bacteria developed
drug-resistant. Western medicine is basically no effect to
virus diseases. There are a lot of side effects of Western
medicine. The patients suffered from a lot of troubles, such
as poor sleep, anxiety, various pan, chronic fatigue,
disorder in menstruation..., but no positive finding in exam
or lab test to establish which disease it is, so no way to
solve it. However, all of these conditions are the dominated
disease/disorder for Traditional Chinese medicine to solve.
The theory that acupuncture is only a placebo effect cannot
explain many clinic phenomenons. For example, in clinic, it
is quite common that in the beginning when a patient came
for acupuncture, the patient feared acupuncture needle very
much for possible pain. Upon acupuncture, the patient may
shake body. Will such fear affect overall healing effect of
acupuncture? It seems not. Our experience is that, after
acupuncture, their pain will also be reduced, so that they
are willing to continue with more sessions of acupuncture.
If the acupuncture is placebo effect, then the fear to
acupuncture should have a nocebo effect. How such nocebo
effect does not really block the healing effect by
acupuncture?
Another example is: a patient has visited several
acupuncturists but the improvement of his disease is not
dramatic. Finally, the patient visited the last
acupuncturist and even did not hold any hope for cure.
However, this time, the improvement is much apparent. How
can we explain that, with the last acupuncturist, when the
patient did not hold any hope for improvement but he got
improvement? Does that mean that a placebo effect not
happened in previous acupuncture clinic at which time the
patient expected very much for healing, but a placebo effect
happened with the latest acupuncturist, though the patient
did not hold any hope for improvement? Does that mean that
the placebo effect is not associated with person’s
expectation and hope?
Similarly, patients have tried Western medicine doctors for
years without any change in their symptoms. After visited an
acupuncture treatment, he got improved a lot. Should we
think that there is no placebo effect during visit to
Western medicine, and the visit to the Western medicine
could even not create a 30%-40% reduction of his symptoms
(the extent that a Western medicine could create due to
trust of patient to Western medicine)? The placebo effect
only happened with acupuncture but not with Western
medicine?
The only explanation is that acupuncture has its own
specific healing effect. The overall healing effect for sure
would be better when the patients strongly believe and trust
the acupuncture therapy to create some level of placebo
effect, but acupuncture has also its own specific healing
effect.
Kavoussi B (2015)
[1154]
also had a review. The data cited and the comment is very
much the same as by Colquhoun D. The former depended more on
a large scale experiments to support his idea, but did not
realize the possible weakness of a large scale experiments
in which the personal skill of acupuncturists were not
ensured enough. e.g. he did not realize the possible bias
due to the variation in personal skill of the
acupuncturists.
Of course, their opinion is disagreed by others. Hennessey S
(2012)
pointed out that "The
placebo has been used to evaluate the benefit of a host of
drugs, but very few studies of accepted interventions or
surgeries are ever done with sham or placebo intervention.
Most studies of interventions are designed without a sham,
and many surgical procedures have never been subjected to
evidence-based rigor. And yet acupuncture is continually
subjected to RCT to prove its efficacy as a valid therapy.
By its nature any sham intervention or surgery has the
potential to create patient bias. The sham or placebo effect
is deeply influenced by expectation, branding, and any other
kind of hype, easily creating participant bias. Acupuncture,
along with surgery, and tech devices are all big generators
of hype and expectation.
Meta-analysis of acupuncture studies suggests that the sham
treatment adopted by acupuncturists may not be the most
effective way to demonstrate the benefits of true
acupuncture. Sham acupuncture may function as an ‘active
placebo’, diminishing the effect of true acupuncture.
Acupuncturists might do better to choose an objective
measurement as convincing evidence, rather than a subjective
symptom such as pain relief, quality of life, etc.
Subjective symptoms can be the hostage of expectation, other
influences, or bias. Perhaps, brain imaging, a chemical
marker, or a comparison of outcomes of procedures used to
treat same conditions should be the indicator for the effect
of true acupuncture, rather than a study form designed to
measure the efficacy of a pharmaceutical drug. "
Based on others studies (Berm BM 2004),
[1071]
Hennessey S
thought that acupuncture treatment may need acupuncture
stimulation doses (with longer times of treatment and more
times of treatment), could the specific healing effect of
acupuncture separated from the placebo effect. He stated
that “Investigators
concluded that (for the
treatment of asthma)
at least 30 sessions in 3 months should be offered to have
an effect, followed by 10 more sessions per year to prevent
a relapse. The extensive treatment with acupuncture could
explain the lack of effect seen in other studies.”
However, as we have been discussed, the treatment schedule
used in the Bern BM (2004) study is a typical Western
acupuncture: acupuncture twice a week for 8 weeks, then once
a week for 2 weeks, again once every other week for 4 weeks.
The treatment frequency is too low.
Horn B
(2011)
[353]
stated that the misuse of sham
controls in examining the efficacy or effectiveness of
Complementary and Alternative Medicine has created numerous
problems. The theoretical justification for incorporating a
sham is questionable. The sham does not improve our control
of bias and leads to relativistic data that, in most
instances, has no appropriate interpretation with regards to
treatment efficacy. Even the concept of a sham or placebo
control in an efficacy trial is inherently paradoxical.
Therefore, it is prudent to re-examine how we view sham
controls in the context of medical research. Extreme caution
should be used in giving weight to any sham-controlled study
claiming to establish efficacy or safety.
Linde K (2010) [417]
pointed out that:
"Sham acupuncture interventions are often associated with
moderately large nonspecific effects, which could make it
difficult to detect small additional specific effects.
Compared to inert placebo interventions, effects associated
with sham acupuncture might be larger, which would have
considerable implications for the design and interpretation
of clinical trials. Total effects of acupuncture
interventions including both specific and nonspecific
effects often seem to be at least moderate in size. We
believe that there has to be a discussion involving
scientists, decision makers, health care providers and
patients whether and when the evidence for clinically
relevant total effects from non-blinded comparisons is
sufficient to consider a treatment effective, even if
specific effects due to the postulated mechanism of action
might be minor or even nonexistent."
Brief summary:
(1). Because there are large amount of positive and negative
data to support or to deny acupuncture as a useful therapy,
the conclusion and opinions by researchers in the Western
countries are also largely variable. Neither side can
convince another. So far, the positive and negative studies
are still publishing year by year.
(2). Acupuncture researchers in the Western countries seem
to develop a weary to acupuncture study.
Chapter 14. Opinions of acupuncturists in China
吕君玲
(2015)
[1155]
stated that, ... The reasons for the
non-significant difference between the acupuncture and sham
group might be due to the study design. For example, sham
treatment in different studies is different. The sham group
may use non-points, tooth-stick, shallow stimulation, etc.
suggesting that currently there is no all-agreed way of
"sham acupuncture" design. In addition, there is difference
among studies, in parameters in patient involvement,
exclusion, treatment schedule, standard to evaluate the
study results. Therefore, current data cannot be used to
tell if the effect of acupuncture is a placebo effect. It is
urgently needed to set up a study design that matches TCM
basic theory.... Before a proper "sham acupuncture" is
designed, we can change our mind and turn research emphasis
to study acupuncture by comparing it with currently most
advanced therapy."
陈勤
(2008)
[1156]
noticed
that 'there are large difference in the treatment frequency
and the length of treatment courses, between the acupuncture
studies in and out China. Is this difference associated with
the healing effect? Currently no study tells how long
healing it may last for the effect of the acupuncture
treatment in each individual disease condition. However,
induced from our study here, the healing effect of migraine
by acupuncture would start to subside after 24 hours. So,
deduced from this, long time in between an acupuncture
treatment is not good to accumulate the healing effect and
to maintain it. Another difference between studies in and
out China is that it is allowed for patients to continue use
of pain killer in most studies. This cannot exclude that the
patients continued the use of pain killer by themselves at
home. Studies out of China mostly compare acupuncture with
sham group. To ensure the quality of the study, the study is
double-blind and mostly use shallow needle in the sham
group. But there is data suggesting that the healing effect
from a shallow insertion group is significantly different
from a waiting group. So, before it becomes clear for the
mechanism of the shallow insertion acupuncture, it is not
suitable to be used as a sham. '
鲍金英
(2015)
[1157]
studied that data on the treatment of
migraine by acupuncture in and out China, pointed out
various factors that a researcher should be aware to pay
attention, but did not mention that the researchers should
also pay attention to the treatment frequency.
刘京
(2007)
[1158]
noticed that the acupuncture studies in the Western
countries usually are with a sham group but not so in
acupuncture studies in China. He believed that current sham
design does not meet the special need for acupuncture study.
He pointed out that: in year 2000, in the world medicine
conference and in its modified version of "Ethical principle
for biological medical study in human being", it was stated
that when test a new therapy, it should be compared with the
current most effective therapy, though it is not exclude the
comparison with a sham therapy, but the sham therapy is used
if there is no effective therapy available. This principle
is suitable to be a reference when design acupuncture study.
刘京
(2007)
commented: in acupuncture study, we can continue the design
of proper sham group for acupuncture comparison, but the
data from traditional sham or a pseudo-acupuncture should
not be used as absolute evidence to make a conclusion. Also,
the studies that did not involving a sham group should not
be regarded as "not scientific" or "not reliable.”
王京京
(2009) think
that, among the negative acupuncture studies in the Western
countries, the most powerful ones are the tree articles;
Lind K (2005), Diener HC (2006) and Alecrim-Andrade J
(2006). The most difference between these three studies and
the positive studies are the design of the sham group.
Currently, the most popular sham acupuncture groups are
using non-point, shallow stimulation, or non-insertion of
needles. However, any of such sham group has its own
disadvantage and none can reach complete placebo effect.
王永洲
(2012)
[1159]
think that, the current acupuncture studies did not follow
the tradition of Chinese medicine of its body-mind coexist
theory, to separate the biological effect from emotional
effect of acupuncture. It also is against the current new
biology-emotion-society model of medicine. No need to stick
to the Western medicine model of separating body and mind
apart. It is still premature to use a sham group as a
comparison. It should not be used as model of acupuncture
study.
王永洲
agreed to make comparison, as suggested by Chinese
Acupuncture Journal, firstly with current conventional
medicine, the current most effective therapy, so find out
the advantage and disadvantage of acupuncture. This might be
more realistic and useful.
田小平
(2008)
[1160]
analyzed
the non-point sham studies in the Western countries and
believed that the weakness of these sham groups are: (1),
the way of choosing the non-points were not standardized
even for the study of the same disease. The way of choosing
point or non-point does not meet the acupuncture meridian
theory. (2), more emphasized on local effect of acupuncture,
not the whole body effect. Mostly compare the acupuncture
points with non-points, less to compare the overall and
comprehensive effect of acupuncture. (3), rarely have
studies of high quality and of large scale size. For many
studies, the study design is not careful, such as small
sample size, unclear the way of random allocation, not
proper disease for acupuncture treatment, not explain in
detail the way of acupuncture manipulation, not sensitive
index was used to evaluate healing results, etc. All of
these make it impossible to reflect the whole body
adjustment or re-balance effect of the acupuncture. The
comparison between the acupuncture group and the sham group
in the healing effect is non-comparable, so that the
conclusion of the studies is not credible.
李春华
(2013)
[1161]
stated that currently there is no standard way to choose a
non-points in acupuncture studies. In China, the non-points
are usually chosen the point about 0.5-1 cm apart of a
typical acupuncture point, or the middle spot between two
acupuncture meridians. From the point of anatomy, it is not
reasonable to choose non-points beside acupuncture spot, and
the non-points in between the two meridians, though for sure
not on the meridians, but if the two meridians are too
close, the non-point chosen would work similar to the
acupuncture point.
杨明晓
(2015)
[789]
specifically
tested and analyzed the article by Hinman RS (2014). Hinman
randomly allocated 282 patients with chronic knee arthritis
into four groups: acupuncture group, Laser group, sham
laser, and non-treatment group. Among several possible
weakness in the Hinman study, the Chinese acupuncturist
pointed that, the patients in the acupuncture group is with
longer term of this disease than in other groups. The
acupuncture was not aimed to stimulate out the Deqi
acupuncture sensation. These could be the main reason that
the study did not find significant difference between the
acupuncture and sham group.
Our comments to the Hinman study are: actually, the
acupuncture in the Hinman study is also once or twice a week
for 12 weeks (totally 8-12 sessions). The Chinese
acupuncturist apparently did not notice that this could be
the main, or an additional main reason for failure of the
study. This is because, if the low healing effect is only
due to the not Deqi, the laser stimulation should also
produce higher healing effect than sham laser and than the
non-treatment group. Actually, even the laser group did not
produce significant improvement than the two comparing
groups. Therefore, low treatment frequency might be the
major reason for the failure of the Hinman study.
项燕
(2012)
[1162] thought
that the critical reason for the failure of acupuncture
studies in the Western countries, is that acupuncturists in
the Western countries do not really understand the meaning
of "conducting meridian and balancing Qi and Blood".
Li
DZ (2014)
[1163]
analyzed articles published in the Western countries up to
2012 about acupuncture treatment of primary hypertension.
They collected totally 2407 articles and among them, they
found only 4 so called high quality articles. The conclusion
of these articles is that acupuncture, when used alone, can
reduce diastolic pressure, but only together with medicine,
could also reduce systolic pressure. However, many articles
published in China showed that acupuncture alone can reduce
both systolic and diastolic pressure, and the extent of the
reduction is much larger than reported in these 4 articles.
The author believed that, the main reason for the less
favorite results from Western countries is not due to what
kind of sham groups used (inserted or not inserted), but due
to low treatment frequency (once or twice a week) and the
less total sessions (only 6 to 10 weeks), because there is
study showing that, acupuncture five sessions per week for
12 weeks can dramatically reduce blood systolic and
diastolic pressure.
李享
(2014)
[1164]
believed
that the reasons for the failure in acupuncture studies in
the Western countries is that they do not really understand
the meaning of TCM theory; do no choose the non-points
carefully and reasonably; did not following the TCM
acupuncture principle of "even the acupuncture point chosen
is not exactly correct, the meridian chosen and touch should
be followed exactly"; the non-points chosen did not avoid
the meridian pathway. In addition, in acupuncture treatment
by acupuncture either in and out China, researchers did not
consider the classification of the hypertension according to
TCM theory.
Liu WH (2015)
analyzed 17
negative articles and 23 positive articles. The author said
that it is not proper to include moxibustion, wrist press
into the evaluation of healing effect by acupuncture; not
proper to let women who have no medical knowledge to perform
finger press at home. In addition, the author pointed out
that there is NO clear difference in the methodology used
for acupuncture study in and out China. The difference in
the methodology is not the main reason for the difference in
study results. However, in each study, there is more or less
weakness, for example, improper choose of acupuncture
points, the uneven personal skill of acupuncturists, no
attention to induce Deqi sensation, too low treatment
frequency, or improper design of the sham or control groups.
郝洋
(2014)
[1165]
reported that, to standardize the study design, and to
properly report study results, are still the urgent aspect
in acupuncture study for acupuncturist all over the world.
They analyzed 10 negative articles and found that there is
no statistically significant in the methodology (Jadad
score) between the negative studies and positive studies.
But there are some weakness in the negative articles in
detail: such as the treatment is not proper; did not follow
the TCM diagnosis to separate a disease into different
subgroups according to TCM theory; the acupuncture points
chosen is not proper, did not pay attention to Deqi
sensation; did not control the personal skill of
acupuncturists in the study; too low frequency of
acupuncture treatment; and the sham is not properly
designed.
毛文超
(2013)
[1166] stated that, the reasons for small difference in the healing
effect between the acupuncture group and the sham group
could be due to weakness in methodology. The weaknesses are:
the treatment plan is not proper; too small sample size;
improper randomization; the standard for inclusion and
exclusion of patients, and that for evaluating study
results, is not clear; improper way of blindness; too short
follow-up period; and improper way of statistic analyses,
etc.
李永明
(2013)
[1167]
proposed a "broad point theory" to explain why in clinic
studies, to stimulate a body surface that does not belong to
traditional acupuncture points but can also show some level
of healing effect. He stated that "everywhere of the body
surface is acupuncture points" might be an overly and
generally a biological phenomenon. That means: to stimulate
any part of the body could produce some kind of
biophysiological reaction of the body to produce a healing
effect. The acupuncture point is a relative point. The
traditional and typical acupuncture point obtains a
relatively stronger such biophysiological reaction than the
nearby non-points. This hypothesis can explain how comes
that, to stimulate acupuncture point or non-point can both
show clinically healing effect. ... Acupuncturists in the
Western countries mostly use thin needles, while those in
China use thick needles. The intensity of the stimulation by
the thin and soft needle is less than the thick needles. The
thin-soft needle may even enhance the placebo effect, so
that it is hard to verified significant difference in the
healing effect between acupuncture group and the sham group.
This theory might be able to explain the difference in the
acupuncture studies in and out China.
霍蕊莉
(2016)
[1168]
believed that there could be many reasons causing the
failure in acupuncture studies in the Western countries,
such as too long interval between acupuncture treatment and
too small the treatment sessions. They also doubt the way of
acupuncture, in terms of needle depth, nourishing or
depleting technique, the length of needle retention time,
the quality of the acupuncturists in studies, etc. But they
did not discuss in detail or gave examples from the studies
published in the Western countries.
Deng S (2015)
[1169]
stated that
certain
problems observed in acupuncture RCTs also occurred in RCTs
in other fields, including insufficient sample size, high
dropout rates, inadequate follow-up, and randomization. The
study of acupuncture is so complex that specific
methodological challenges are raised, which are frequently
overlooked, including sham interventions, blinding, powerful
placebo effects (even stronger than an inert pill) and
variations in acupuncture administration. The aforementioned
problems may contribute to bias, and researchers
systematically attempt to solve these problems.
Apparently, only small number of the acupuncturists,
questioned that the low treatment frequency of acupuncture
might be the major reason for low healing effect in the
acupuncture group, that again is the major reason to cause
the non-significant between acupuncture group and sham group
in the acupuncture studies in the Western countries.
Most of the acupuncturists in China apparently do not accept
the fact that there could be a kind of placebo effect in
clinic study and work. They explained and focused on the
sham group as improperly designed and used. They tended to
accept the idea to compare acupuncture with currently most
effective therapy for a given disease. They cannot explain
the possible discomfiture if the current "effective therapy"
is also a placebo effect.
[1170]
Brief summary:
(1). Acupuncturists in China seemed hesitated to accept that
there could be a placebo effect during acupuncture
treatment, which can be as higher as to affect the
comparison in the healing effect between an acupuncture
treatment and a sham treatment.
(2). Most of them do not accept the current way of design
for a sham group. They think that the current sham group is
not a proper sham to test acupuncture healing effect.
(3). Only a small number of acupuncturists in China believe
that the major reason for the failure in acupuncture studies
in Western countries is due to low acupuncture treatment
frequency and less total acupuncture sessions in the Western
countries.
Chapter 15. Our own comments
15.1. Selection of acupuncturist
In the acupuncture clinic research,
one of the most important parts is acupuncturist for his/her
personal skill in acupuncture treatment. If the personal
skill of an acupuncturist is poor, there will be very higher
chance to fail in the study.
We recommend having a selection
process for a proper candidate of acupuncturist. All the
acupuncturist to use his/her actual way of acupuncture
treatment in the clinic, such as the use of acupuncture,
cupping, moxibustion, fire-needle, auricular
acupuncture/pressure, TDP lamp, etc., and allow the
acupuncturist to decide the way of acupuncture, including
the acupuncture points, the number of needle, the frequency
of the treatment, to see if the acupuncturist can improve
the symptom (in non-specific low back pain) by more than 55%
(giving 20 patients), or by more than 85% of the healing
effect reported in literature for the same disease by others
[26].
If the healing effect cannot come to such level, the
acupuncturist is not suitable to be involved in acupuncture
clinic study, regardless of how many year the acupuncturist
has been in clinic work.
15.2. Special acupuncture study
Special acupuncture study means to test if acupuncture is
placebo effect or not. This is urgent question for
acupuncture researchers in the Western countries. The
simplest way to test it is to have acupuncture in general
anesthesia (start acupuncture after the induction of the
general anesthesia). It can be tested for the treatment of
coma, shock, persistent vegetative state, or dementia, but
the treatment of such conditions needs higher personal skill
of an acupuncturist.
For study in these conditions, it is no longer significant
to have a sham group. It is also impossible to get agreement
for the patient before the acupuncture. It will have no
drop-off cases either.
15.3. Ordinary acupuncture study
For ordinary acupuncture studies, we recommend the
researcher could consider the following:
15.3.1. Wash-up phase
Have a wash-up phase. To give patients a sham treatment for
3-4 weeks with the same treatment frequency as the following
true study phase. Better to have the sham acupuncture once a
day, 5 days per week, for 3-4 week.[527,528,550,1171-1173]
Exclude those of patients who had symptoms reduced by more
than 30%. These patients belong to placebo-sensitive
patients. They are not good candidates to test the healing
effect of any therapy (inducing new drugs, surgery,
chiropractic, or physiotherapy, etc.). These
placebo-sensitive patients can be given true acupuncture
parallel to those who will come into the following study
phase, but the data in this group is not the primary aim of
the study.
Those of patients who did not have more than 30% reduction
in their symptoms can be treated with true or sham
acupuncture in study phase (acupuncture phase).
15.3.2. No-treatment group
Depending on the aim of the study, this group may or may not
be omitted.
If the primary aim is to test if the acupuncture group is
better than a sham group, this no-treatment can be omitted
as for most clinic studies.
However, if we want to know exactly how much effect of a
placebo effect in a sham group, the no-treatment group has
to be included. This is because that the healing effect from
a sham group contains placebo effect, natural turn-over, and
regression-to-normal, etc.
15.3.3. Sham group
The difference between the acupuncture group and the sham
group should be that there is acupuncture performance in the
former but not in the later.
Current data strongly suggest that the failure of
acupuncture study is due to the poor healing effect in the
acupuncture group, rather than the kinds of sham group used.
Therefore, either inserted or non-inserted sham group can be
used under the condition that the acupuncture and the sham
acupuncture are performed once a day, 5 days per week, for
more than 20 sessions (depending on the disease to study).
The advantage of insert-needle sham group (shallowly
inserted needle on non-points or other-points) over
non-inserted sham groups is that the procedure much closely
mimics to verum acupuncture procedure. Even a person had
previous experience with acupuncture treatment may be hard
to tell the insert sham group, so it can eliminate the need
to find acupuncture neive paticipants.
15.3.4. Acupuncture group
Only use acupuncture, not use moxibustion, cupping, bleeding
therapy, massage, of Tuina. But allow the acupuncture to
select the acupuncture basic points or special points, the
number of the points during each session, the frequency of
the treatment, and length of each session.
The acupuncture should be performed once a day, 5-6 days per
week, for totally 20-30 days (referring to the way used by
acupuncturists in China for the disease to study) . Allow
the acupuncturists keep the same way of communication with
patients.
[790]
One of the characteristics of Chinese medicine, acupuncture
or herbal therapy, is individual treatment.[1174]
TCM regards each patient differently. This is quite opposite
from Western medicine, which wants to standardize everything
to every patients. Test acupuncture by a Western medicine
way, not change treatment plan according to each patient's
condition, might be one of reasons for the failure of many
acupuncture studies. It could also be one of the importance
reasons for high fall-off rate in acupuncture studies in the
Western countries. For example, if a patient cannot tolerate
10 needles each time, or cannot tolerate the intensity of
the needle stimulation as it is previously designed, but we
insist to do it, the patient will have no way but escape.
The stimulation of acupuncture in each session is also very
important but it is hard to standardize the stimulation dose
among each session and among acupuncturists. We recommend
using E-acupuncture, especially in large scale acupuncture
studies.
15.3.5. Location of study
We recommend having acupuncture study in China first. This
is because the large population in China. It is easy to
collect sufficient number of patients to participate the
study, as to be able to finish the study within a short
time. Anyway the acupuncture is developed in China.
Acupuncturists in China have responsibility to show the real
healing effect of acupuncture to the world. If the study is
indeed positive, than transfer the study to the Western
countries. If the acupuncturists are from the Western
countries,
[27]
we have to question the personal skill of the acupuncturist,
among other possible reasons.
15.3.6. Monitor or Supervisor
The acupuncture should be performed by professional
acupuncturist but need supervisor and monitor by some
researchers who currently do not believe acupuncture
specific effect. If it is performed by those people whose
profession is not pure acupuncturist, the result of the
study is largely questionable. If it is performed and
finished all by acupuncturist, the result should be more
credible, but the data treatment might be questionable.
Monitored by those who do not believe acupuncture, the data
would be more credited. By this way, it only needs to blind
the patient, not the acupuncturist, or the data analyzers.
As pointed out by others, that it is impossible to blind the
acupuncturist. The feasibility to have a monitor is that
there are already some researchers1
who do not believe acupuncture.
As we discussed, this should be an internationally observed
study about acupuncture to finally answer if acupuncture is
placebo effect or not. We should invite both the acupuncture
experts from China and those from the Western countries who
do not believe acupuncture, to finish the study, and report
it in an international conference.
After established that acupuncture is not a placebo effect,
the setup of a monitor can be omitted.
15.3.7.
Acupuncturist recommended
It is needed to invite acupuncture experts to participate
the international acupuncture study, so as to make sure that
any failure from the study is not due to quality of the
acupuncturist for his poor personal acupuncture skill. Any
acupuncture study should not only convince acupuncturists
and researchers in the Western countries but also those in
China. If with the participation of the well-recognized
acupuncturists from China, the study is still failed, we all
will accept that acupuncture is indeed a placebo effect. We
stop the acupuncture and discontinue any more studies on
acupuncture.
At least, we can recommend the following experts:
[28]
professor
石学敏,梁繁荣教授;吕景山教授;韦立富教授;方剑乔教授;张道宗教授;张侬教授;王升旭教授;方晓丽教授;纪青山教授;
石印玉,
and so on.
Of course we cannot invite expert level of acupuncturists to
participate every acupuncture study, but we need a scale to
know what the highest healing effect is, by acupuncture in
the current time, and then to know what is the average level
for local acupuncturist. They are not the same meaning. If
the healing effect of the local acupuncturists is too low,
even if I am also an acupuncturist, I would not argue if an
insurance company does not reimburse the cost for
acupuncture treatment.
Therefore, we need acupuncture experts to participate the
acupuncture study, so as to give a clear answer to the
question if acupuncture is merely a placebo effect, a
question which should have not been a question to
acupuncturists in China.
15.8. Multiple study locations
For the treatment of an ordinary disease by Western
medicine, once the diagnosis is established, the treatment
would be pretty much the same no matter it is in New York,
or in Vancouver. But for Chinese medicine, it may not be so.
The personal ability of practitioners in Chinese medicine,
acupuncture or herbal therapy, is largely variable. If one
TCM doctor cannot solve the disease, it does not mean that
another TCM doctor cannot either. This is reality.
To solve the variation among acupuncturists from different
clinic locations, one way is to test their personal skill
before or during experiment (such as with the clinic group).
Another way is to allow the use of electrical acupuncture or
warm acupuncture, so as to standard the stimulation in each
acupuncture session.
[29]
Of course, the electrical acupuncture is not the traditional
acupuncture. But if with the electrical acupuncture, the
healing effect is not reasonably high, it would be
hardly expected that with manual acupuncture the healing
effect would be higher (for most of acupuncturist).
Instead of designing a large scale study involving more
clinic locations, we would recommend to finish the large
scale experiment in a single location by a given and limited
number of acupuncture experts. This is not difficult in
China.
15.2.6. Goal of future acupuncture study
There are several remaining questions in acupuncture study
that we need to answer one after another:
(1). If acupuncture is a placebo effect? If it is not a
placebo, can we omit it in future study? Can we then compare
the acupuncture group with the currently most effective
therapy and accept it if it works equal or better than the
compared therapy?
(2). How can we trust the healing result from a study in
which the healing effect of the sham group (e.g. the placebo
effect) is high? Should we think about to involve a
credibility index in evaluate the quality of a study? Sham
group with higher healing effect should get higher
credibility than that with lower healing effect?
(3). How to evaluate the amount of placebo in a group of
combined therapies, such as acupuncture group (which include
a healing effect due to the placebo and to specific
acupuncture effect), or a group with acupuncture plus
physiotherapy (the total placebo effect in the combined
group should be considered the same, doubled, or triples of
that in the single sham group)?
(4). Difference in
susceptibility rate of
placebo in different nations, especially such in Germany,
since most of the negative studies seemed from there. The
susceptibility of placebo is negatively related to amount of
the specific healing effect of acupuncture.
(5). Difference in incidence rate of along-meridian feeling
in different nations. The along-meridian feeling is
positively related to the healing effect of acupuncture.
All of these questions are closely related to future
acupuncture studies and need to be clarified.
Brief summary:
To answer if acupuncture is placebo effect, we recommend
having an international cooperated study, involving both
acupuncture researchers from Western countries and
acupuncture experts from China. Best way is to start the
study in China, to study the effect of acupuncture during
general anesthesia. This is also the easiest way and
quickest way to answer this question.
Chapter 16. Difficulty in acupuncture study
Now, we can make a comparison between acupuncture clinic
study and Western drug clinic study. In the clinic drug
study, the shape, size, and the color of sham drug to study
can be made the same as the true drug. It is hard for
patient to verify between the true and the sham durg
tablets. Such true and sham drug can be produced in large
scale and be used to thousands of patients the same time and
in different part of the world.
However in the clinic acupuncture study, most of the
non-inserted sham groups have more or less difference to the
verum acupuncture group, except possibly for inserted sham
group, in the way of operation of the treatment. The dose of
stimulation of the acupuncture group could be different from
session to session (even by the same acupuncturist). The
dose of such stimulation can also be different among
different acupuncturists. Therefore the efficiency of
acupuncture treatment is largely variable from session to
session, and from acupuncturist to acupuncturist.
There are data suggest that sham acupuncture might induce
more placebo effect (enhanced placebo effect) than placebo
pills (may be because the sham acupuncture belongs to
action-type hint process). The placebo effect in the verum
acupuncture group might be higher than the sham acupuncture
group (due to the pain feeling, that might induce stronger
and enhanced placebo effect), or less than the sham
acupuncture group (due to fear to pain induced by needles).
Therefore the relationship between the verum acupuncture and
the sham acupuncture are unstable and variable.
If
the relationship of the factors in the medical study can be
regarded as patient-medicine (and or placebo pill)-doctor,
the relationship in the acupuncture study would be
patient-acupuncture (and or sham acupuncture)-doctor. The
acupuncture (and or sham acupuncture) would be the same
position as the medicine (and or placebo pill). The medicine
(and or placebo pill) can be regarded as fixed and under
controlled factor, the acupuncture (and or sham acupuncture)
is not at all a fixed and under controlled factor.
Therefore, the clinic study of
acupuncture is more difficult and more complex than that of
medicine. Currently, no matter how much the healing effect
obtained in the acupuncture group, it is regarded as the
normal and accepted healing effect of acupuncture. Rarely is
it questioned as the failure of acupuncture group.
Chapter 17. Conclusion
We, from a clinic acupuncturist point of view, reviewed the
current data about acupuncture and tried to see the possible
reason(s) that may bring out a comment that acupuncture is a
placebo effect.
We found that:
(1), the healing effect of a sham group in the Western
countries, is as average 23%, while that in acupuncture
group is about 35%.
(2), acupuncture in the Western countries is mostly once or
twice a week for less than 12 times.
(3). the healing effect in the sham group in China is about
23% too, but that in the acupuncture group is more than 50%
or more.
(4).
Acupuncture in China is mostly once a day, 5-6 sessions a
week, for more than 10 sessions (usually more than 15-20
sessions). Apparently in the Western, the acupuncture
stimulation is lower and healing effect is lower too, while
the stimulation dose is higher and healing effect is also
higher in China.
Current data suggest that, with higher stimulation dose, the
healing effect of sham group tends to be lower but that of
acupuncture group, higher, so as it tends to yield a
positive result about acupuncture study. Therefore, we
predict that the reason(s) for the failure of acupuncture
studies in the Western countries is at least originally due
to low treatment frequency and lower dose of stimulation of
acupuncture. Under the high treatment frequency, there is no
major difference between the inserted or non-inserted sham
groups in the extent of healing effect.
The direct evidence support that acupuncture is not a
placebo effect is the treatment of acupuncture in patients
with coma, shock, persistent vegetative state, and during
and after anesthesia, in which the patients are with no
consciousness or very weak consciousness, so as not being
able to produce a placebo effect. Such disease conditions
are very rarely studied in the Western countries.
Further evidence is that acupuncture can also work for
dementia patients. In addition, with high treatment
frequency, it is significantly difference in the healing
effects between different acupuncture points, between the
acupuncture points and non-points, between different ways of
acupuncture.
Moreover, acupuncture can well work for young children and
for animals. Both should be hardly affected by a hint
(placebo influence). Especially when the acupuncture is only
one time and the conditioning reaction cannot be established
among them.
The healing effects of sham groups are a largely broad rang.
This means that the susceptibility of people to a hint (sham
treatment) is largely variable, and in reality there are
both high and low susceptibility people. To test if any
therapy, including new drug, surgery, physiotherapy,
chiropractic, as well as acupuncture, the placebo effect
should be excluded. One of the ways to exclude the placebo
effect from the acupuncture treatment is to have a pre-test
phase, in which to give patient a sham treatment for 3-4
weeks, and exclude those of patients who have their symptoms
reduced more than 30% (not up to 50%). This means to test
specific healing effect of any therapy among placebo
non-sensitive patients.
Beside the weakness of acupuncture studies in the Western
countries as above, there are several other weaknesses: (1),
to fix acupuncture treatment plan to all the patients
without any variation according to patient individual need;
(2), limit the communication between the acupuncturist and
patients, so makes it impossible for the acupuncturist to
change treatment plan according to the variation of the
disease severity and the need of the patient personal
conditions; (3), the acupuncture operators are in a large
part not professional acupuncturists. The personal skill is
questionable.
Because the poor healing effect (improper study design
and/or poor personal skill), acupuncture researchers in the
Western countries rarely study objective indexed diseases,
not to speak of the severe conditions, such as coma, shock,
persistent vegetative state, post-stroke syndrome, bell
paralysis, etc., so that leave an impression that
acupuncture can only be used to treat subjective diseases,
such as pain. This again enhances the suspect that
acupuncture is a placebo effect.
To prevent the mutual distrust between the acupuncturists in
and out China, we suggest to have an international
cooperated study on acupuncture, by involving acupuncture
researchers from Western countries and acupuncture experts
from China, so to answer the question permanently if
acupuncture is a placebo effect or not.
Acupuncture needs to go ahead and not stands at the same
spot, or goes around and around.
Chapter 18. Several comments and explanations
1. The reaction to a treatment for a healthy people and a
sick people might not be the same,[1175,1176]
so we try not to use data deduced from healthy volunteers.
For the same reason, we tried also not to use data from a
lab healthy animal.
2. Generally speaking, for the treatment of an acute
disease, one time treatment with acupuncture is possible,
especially by an acupuncture expert. But for most of
acupuncturists and for most of chronic diseases, they need
more times of acupuncture treatments. Therefore, we do not
include the data of only one time acupuncture (except the
data for the treatment of nausea).
3. We paid more attention to the healing effect when the
healing plan finished. Very rarely is there a disease which
did not get better at the end of the treatment course but
better several months or years after the stop of acupuncture
courses. The healing effect after stop of acupuncture could
be largely variable due to many reasons, especially if this
disease has not been brought to a cure or near cure status.
So, we choose the data just after finish of the acupuncture
treatment plan.
4. Principally, we do not include the data by a TCM master
student or doctoral student. Acupuncture is a healing
technique highly dependent on personal skill. The
credibility of data by people in student period is not as
high as that in clinic practice period. However, we include
their review data.
3. We paid more attention to the healing effect when the
healing plan finished. Very rarely is there a disease which
did not get better at the end of the treatment course but
better several months or years after the stop of acupuncture
courses. The healing effect after stop of acupuncture could
be largely variable due to many reasons, especially if this
disease has not been brought to a cure or near cure status.
So, we choose the data just after finish of the acupuncture
treatment plan.
6. We look at the data from the point view of an acupuncture
clinic practitioner. This is not a strict review paper. We
did not have statistical analysis of our data yet, since the
data collected here is extremely largely variable for many
aspects, which makes the statistical analysis less
meaningful.
All the comparisons here are for the use of later
professional researchers for a reference. We only paid
attention to the overall healing effect of acupuncture in
and out China, and how the acupuncture was performed
generally by acupuncturists in and out of China. What we did
seems as a much larger size "regression analysis,” a "smear
analysis,” or a "non-linear regression analysis.”
7. Data from Hong Kong are in most cases different from
that in mainland of China for experiment design and more, so
they are included in the "Western countries.” No any
political meaning for us to do so.
8. Thanks very much for internet, for Google, Medline, BJM,
Research Gate, CNKI.net, and Wan fang Med Online. We look
the world on the shoulder of a giant.
Chapter19. Consideration and suggestion for future medical
service system
It is well known that, no matter it is in China or in the
Western worlds; the cost for healthcare occupies more and
more the GDP part. Theoretically, the current medical
services are much more advanced than that hundreds of years
ago. Indeed, the life span of the population is increased.
However, the number of the sick elderly is also more and
more, since more and more people live longer due to their
long term intake of the medicine. One way to explain this
phenomenon is that current medicine saved life-threatening
diseases and emergency conditions for sure, but fails to
solve chronic disease or the diseases from which they saved.
Many acute diseases and emergency diseases became chronic
disease later (such as persistent vegetative state). Once a
disease cannot be cured by a surgical operation treatment,
it would be hard to solve by an internal medicine as well:
chronic just mean that it is hard to cure. So, the disease
can come again and again and the patients need to take
medicine again and again, and so that the healthcare cost
goes up sharply. In addition to the increase in the payment
to pension to more population that comes into old age, the
burden from healthcare would soon or later crash the whole
national social service system.
How to solve
this problem? Can we depend on the current Western medical
system? The current situation happens when the Western
medicine has been in authority and dominated. Its history
has already showed and proven that it cannot solve all of
these problems. It is also hardly to see glimmers of hope on
the horizon for future.
According to our own understanding to the Western medicine
and Chinese medicine, we believe that the best way to solve
this problem is to adapt both Western medicine and Chinese
medicine. This idea is to let the Western medicine do what
they can do best: surgical operation and allow Chinese
medicine to solve most of the chronic diseases, unless it is
also hard for the Chinese medicine to solve the diseases
concerned.
Chinese medicine includes, at least, the herbal therapy and
the acupuncture therapy. Among the various therapies in
Chinese medicine, the herbal therapy is apparently the major
therapy actually. Of course, the final healing effect of the
herbal therapy depends on the personal skill of the
herbalist and that of the acupuncture depends on the
personal skill of the acupuncturist. For some kinds of
diseases, acupuncture might work better than acupuncture.
Our idea is: for the following conditions let the Western
medicine to work first: any disease that can be for surely
cured with surgical operation.
If the disease cannot be cured by the surgical operation, if
it normally needs the patient to take medicine almost
forever, if the patient is also prescribed for pain-killer,
sleeping pill or sedative for the treatment; or if the
diagnosis is uncertain, but the patient suffers much from
discomfort, it is better to see if Chinese medicine can
work, such as most of chronic diseases, except of some that
might also be hard for the Chinese medicine (e.g. Cancer,
AIDS, etc.).[30]
The goodness is that there are already a large number of
acupuncturists in most cities in the US and Canada. For
example in Edmonton, Canada, the population is 870000, while
there are at least 250 acupuncturists in the city. It means
that every 3480 population is with one acupuncturist. This
number is much higher than that in China: at least
1300,000,000 populations are associated with about 270000
Chinese medicine doctor (among them, most is herbalists, not
acupuncturists). This means that every 48000 Chinese is
associated with one Chinese medicine doctor.
The weakness so far is that most of the acupuncturists in
the Western countries do not use herbal therapy. Or they
only use simple herbal patch, herbal oil, or herbal pill for
the treatment. The healing effect of these easily-use herbal
products is limited somehow, compared with typical oral
herbal therapy. With update of their herbal therapy skill,
the overall healing effect should be much higher than it is
now.
Return to
Chapter 1 to 5
Reference 1-510
Reference 511-1048
Attached
list 1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
18a,18b,18c,19a,19b,
19c,
20a,
20b,20c,
20d,
21a,
21b,
21c,
22,
23a,
23b,
23c
|
|
|